 |
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
 |
 |
 |
Régions du Québec |  |
 |
 |
|
 |
 |
|
 |
 |
|
 |
 |
 |
 |
 |
 |
Rubriques |  |
 |
 |
|
 |
 |
|
 |
|
 |
 |
 |
The Arlene Berry Story | 2011 Update
There is a public interest in knowing how Arlene Berry came to her death and how her health care providers are implicated. There is nothing contained herein that the police could not have uncovered for themselves, had they not been instructed by their superiors not to look further. The reason given by OPP in Kirkland Lake, Ontario for their decline to investigate further, "we have to live here too", suggestive of 'selective enforcement', murder withstanding, and gross dereliction of duty.
The implications of the findings contained herein are so profound that, according to one hospital insider, Health Canada has issued a “gag-order” in an effort to save face (with so many doctors and nurses involved in this unnecessary death), a blatant attempt not only to prevent the media from becoming involved, but also as a means to deny justice. In my opinion the health authorities have also insinuated themselves into a criminal conspiracy, or party accessory (after the fact) to a medical homicide. These political and ministerial thugs, criminals attached to the public purse, there to divert the natural order of things including the sinister College of Physicians and Surgeons of Ontario and their corporate counterparts, the Canadian Medical Protective Association, seem to think that they and the physicians they seek to shield are all above the law. Perhaps its time they had their moral codes thoroughly overhauled via the Internet.
First, know that the medical establishment is guilty of culpable homicide by deception. They have downplayed the threat of medical negligence, iatrogenic injury and death and concealed the evidence for years. “Of all the self-interested policies that created the massive crisis our entire health system faces today,” one commentator writes in New Physician, “perhaps the most devastating has been the medical profession’s evasion of public accountability….” Our system of justice is supposed to protect the public but its all a pack of lies. It seems clear that doctors in Canada are licensed to injure, maim and kill carte-blanche, without accountability.
Published under a wide variety of titles internationally, the Arlene Berry case stands as a testament to what can only be construed as widespread corruption in Canada’s health care system.
In Memory of Arlene Berry 1958-2000
I began this investigation in the early summer of 2000. I have had to study medicine, literally. There have been many obstacles in my path to overcome. Someone in the government or medical profession has gone to a great deal of trouble to discourage my efforts to make my findings public by interrupting and interfering with my various websites and by attempting to block or sabotage my web content for years. You are encouraged to think critically about what you find here. Do your own research if you still have questions.
The FACTS
In December of 1999, Arlene Berry was sent to Timmins & District Hospital in Timmins, Ontario, where she was diagnosed, according to her physician, with “carcinoma of the left main bronchus with residual cancer of the aorta due to a complete collapse of the left lung”. This refers to residual disease, i.e. cancer cells that remain after attempts to remove the cancer have been made.
Her family MD, Dr. Edward. H. Jordan had been treating her assumptively for what he termed to be a “suspected bronchitis”. It took another doctor to read her X-ray chart, and to order more appropriate testing before anything was done. This naturally infuriated the patient prompting her to publicly berate her family MD in front of everyone in the hospital emergency department. According to a hospital insider, she was probably “blacklisted” from that point on.
On or about January 12th of 2000, Arlene Berry was admitted to the Timmins & District Hospital in Timmins, Ontario, where she had a left lung pneumonectomy on January 13th of 2000, under the care of Dr. Claudio de la Rocha, a Cardiovascular and Thoracic Surgeon who immigrated to Canada from Mexico. This doctor has a propensity for selective treatment, including a criminal past history of active and passive euthanasia.
Following surgery, Arlene Berry was discharged home 5 days later. On or about March 16th of 2000, Arlene Berry returned to Timmins where she underwent follow-up study and testing at the same hospital, consisting of a CT scan, and a mediastinoscopy with mediastinotomy, as part of her post-operative evaluation.
What the family had found to be peculiar however, was a dramatic voice change at some point following the mediastinal procedures, suggesting a “partial vocal fold paralysis” thought to have been procedure related. Although she began to regain her voice in the weeks that followed, her voice remained somewhat “whispery” for the remainder of her days. Following that testing, Arlene confided “I don’t have AIDS, or brain tumors, or anything like that, but I might have a “cyst”, or “infection”.
A cyst is a suitcase for the infectious material inside. Some of them parasites with simulation of stroke related damage in cultured human nerve cells have been reported. Stroke-like conditions include speech problems, headache, weakness and dizziness, with or without vision problems. Trapped blood (ie. from an old hemorrhage or occipital bleed) can also lead to the growth of cysts. Patients can be asymptomatic even if the cyst is quite large.
Arlene Berry was then referred to the Northeastern Ontario Regional Cancer Centre situated at the Laurentian Site, Sudbury, Ontario for consideration of radiation therapy under the care of Dr. Hugh Prichard, a radiation oncologist. By the end of April 2000, Arlene Berry had completed her post-operative course of radiation therapy. In light of this treatment, her condition was seen to be stable. She had been scheduled for X-ray follow-up in Sudbury on Tuesday May 30th at 2:30 PM. Sadly, she did not live long enough to meet this appointment.
Following radiation, Arlene Berry developed “flu-like” symptoms suggestive of gastrointestinal illness within two weeks following radiation therapy, at the end of April of 2000. She died on the 24th of May of 2000. Total time lapse 24 days; mean >3 weeks , or just under 4 weeks.
I have given careful consideration to Guillain Barre syndrome (GBS) and its variants. May is Guillain-Barre-Syndome awareness month. The timeline for the disorder definitely fits the bill. GBS can develop over the course of hours or days, or it may take up to 3 to 4 weeks. Most people reach the stage of greatest weakness within the first 2 weeks after symptoms appear. 66% reach nadir in 2 weeks, 92% in 3 weeks; by definition MUST peak by 4 weeks. GBS frequently follows a flu-like illness, or viral syndrome by a week or two, as in this case.. The severity of the condition also varies and sporadic reports have described the occurrence of an acute severe poly-neuropathy leading to a complete ‘locked-in’ syndrome, often "misdiagnosed" as a fatal brainstem event where the clinical picture is also "misinterpreted" as brain death. Misdiagnosis is often the result of incompetence, or gross medical negligence.
According to her Rx scripts, Arlene Berry had been given Amoxicillin for "infection". Amoxicillan belongs to a class of penicillin-like drugs, side effects of which include severe nausea and vomiting, including abdominal pain.
According to the hospital record Arlene Berry was admitted to the Kirkland and District Hospital on May 23rd of 2000 by Dr. Spiller for “IV fluid and Gravol”, evidenced at A-6. According to record, she was given more than IV and Gravol. If not Dr. Spiller, who ordered the 30 mg MS Contin on his watch? MS Contin is a brand of a time-released formulation of morphine sulfate, usually taken every twelve hours for chronic pain. From the record it seems clear that either Dr. Spiller lied, or that he was totally oblivious to the administration of Morphine Sulfate evidenced at A-12. According to the same record, Arlene Berry had been admitted for “vomiting”. Vomiting is not a diagnosis, but rather a symptom of many causes.
A-5 of the record documents the presenting complaint as “headaches, accompanied by severe stomach pain”, and “abdominal pain ongoing for 2 weeks”, for which she had been prescribed “antibiotics”. The key symptom here is actually SEVERE ABDOMINAL PAIN that may be constant, but may also come and go.
Abdominal or stomach pain concurrent with nausea and vomiting points to the abdomen as the source of the problem, which should have been a ‘red flag’ suggesting the possibility of intestinal obstruction. Abdominal pain can also be the result of “intestinal ischemia”. The hallmark of intestinal ischemia is abdominal pain.
OP-53 documents a history of bloody bowel movements when voiding evidenced by “bloody BM’s x 4 days” (bloody, black, or tarry stools). Bloody stools may signify bleeding stomach, diverticular bleeding, or intestinal infection. The same record documents “pale-looking and lethargic”.
Pale skin suggests decreased blood supply to the skin. Blood vessels in the body constrict to conserve blood in the body’s core, making you feel cold and your skin go pale. Lethargy and drowsiness are often associated with moderate to severe dehydration, including congestive heart failure. Lethargy may also be caused by the toxic effects of waste products on brain function.
According to the record at OP-53 she was “Here 1 week ago for UTI. Last period on 6th of May”. Onset of menstrual period is closely related to onset of migraine headaches, including illness. Case reports cited primarily in women having period in which a blood-soaked tampon may provide an excellent breeding ground for the bacteria and is a significant cause of urinary tract infections.
The same record dated May 22nd documents “For 2 weeks had flu, migraines”. Flu symptoms, like headache, fever, chills, stomach pain, usually appear anywhere from 1 to 4 days after a person has been exposed to the flu virus. Migraine headache may also be caused by swelling of blood vessels in the brain, due to increasing pressure. Headaches from the flu can feel a lot like migraines. Influenza is not the same as a stomach flu. This is most likely due to a GI (gastrointestinal) infection, not the flu. Headaches are also common in people with GI trouble. Further, headaches have also been reported in rare cases of GBS.
CAVEAT: Many different types of bacteria and parasites can also cause GI infections, leading to CNS infection. CNS infection can broadly be grouped into meningitis, encephalitis and less commonly cerebral abscesses.
According to the record at A-6, she returned to the ED (emergency department) the following day, on May 23rd of 2000, “with the very same complaints”. Rapid evolution of illness and patient return within 24-48 hours should have been a red-flag in of itself as it suggests a severe illness.
The RN who saw her noted that she had been “taking morphine” for pain management, and also that she had recently “stopped” taking the morphine, noting her recent medical history that for “2 weeks” she had the “flu”. The same record also documents a question mark (?) with respect to possible morphine allergies, seen at A-5.
OP-53 documents a history of Tylenol and Aspirin, including a documented “daughter states takes a lot”, suggests a history of drugs that can break the gastric barrier, and damage the gastric mucosa, ie., NSAID’s (non-steroidal anti-inflammatory drugs). Aspirin is the drug classically associated with Reye syndrome.
According one of her Rx scripts, Arlene Berry had been prescribed sodium phosphate (sometimes used to treat constipation or to help relieve impacted bowels) while under the care of her oncologist, and sodium dosucate, an ionic surfactant used as a stool softener prescribed by her family MD. She had found the prescribed stool-softener to be ineffective and so turned to over the counter laxative and tap water enemas for what appeared be drug opiate induced dysmotility.
CAVEAT: Enema is contraindicated in patients with fulminant disease, because of the danger of precipitating toxic megacolon or perforation of the colon. Unfortunately, the health care providers who attended to this patient failed miserably to educate or instruct her in helpful ways, as to the “Do’s & Don’ts”, and also as regards the dangers of the drugs and treatment she was given. I know for a fact that she had been severely constipated at one point and that “megacolon” was a factor, only I didn’t know what it was at the time.
What appears to be a referral at A-6 of the medical record, a chart-copy from the admitting physician, Dr. Spiller, directed to the attention of the family physician, Dr. Jordan, documents what I take to be a provisional diagnosis of “vomiting”, and “vomiting, lung CA” documented at A-11.
According to Dr. Jordan, “she had presented to the ED several days before with vomiting and it was thought that she had a UTI”, to rule out delay in seeking treatment. According to the hospital record at A-8 “she was given antibiotics and sent home”.
According to the outpatient record at OP-54, the patient’s recent head CT scan showed “NO METASTASIS”, and her mediastinoscopy, a surgical procedure to examine the mediastinum inside of the upper chest between and in front of the lungs, were found to be “NEGATIVE”. From that record it seems clear that NO clinically detectable metastasis were found.
The Health Management Record at A-21 of the record documents the patient’s sensory cognitive perceptual pattern as “sedated”. Increased sedation is also a serious side effect of many pharma agents, including electrolyte derangements which can mimic sedative intoxication.
The record at A-23 documents a "slurred speech" as evidenced by a check mark in the upper left corner of that document. With Guillain-Barre syndrome (GBS), speech may be unintelligible, “slurred or whispery" as the various muscles required to form speech are weakened.
The record at OP-54 dated May 22nd of 2000 documents a "haggard appearance", including "large blood trace leukocytes", marked by an unusually high number of WBC’s (white blood cells). An increased number of WBCs is consistent with a central demyelinating inflammatory process suggestive of GBS which has been known to follow influenza infection. Guillain-Barre syndrome (GBS) is an immune-mediated neuropathy in which leukocytes and humoral components of the immune system proposedly initiate localized inflammation.
Facial weakness is also commonly a feature of GBS. Weakness of facial muscles produces a characteristic haggard appearance, or a deceptively disinterested facial expression. The characteristic appearance of a “haggard” or “mournful” face and drooping eyelids is caused by facial muscle paralysis. A sagging mouth or a crooked smile is a part of the same problem.
The Outpatient Record from the hospital dated May 22nd of 2000, seen at OP-54 documents a recent history of “hematuria” (blood in urine) for “three days”. The healthcare provider who saw her made a diagnosis of "UTI". The same record documents a prescription for Cipro, for treatment of “urinary-tract infection”. The belated test result however, what I assume to have been a urology test, or a bacterial culture test, evidenced at OP-55 of the record, later returned a finding of "NO Growth". Caveat: A negative urine test can also suggest the presence of unusual bacteria or viruses causing symptoms of UTI.
The record at OP-54 documents "SEPTRA DS GIVEN BEFORE & CIPRO GIVEN AFTER". The same healthcare provider (whose signature is illegible) also made a notation with respect to the “flu”, which was then directed to the attention of the patient’s family MD, namely, Dr. Jordan.
Cipro is a broad-spectrum antibiotic indicated in the treatment of a variety of infections, including the flu. Bactrim/Septra DS is also the antibiotic most frequently associated with drug-induced aseptic meningitis. Certain combinations of medications, such as penicillin and sulfa-based antibiotics can cause the body’s immune system to react by over-stimulation, sending white blood cells (called T cells) rampaging through the body destroying its own tissues. This is known as an autoimmune disease and can be triggered following a surgical infection, or by a flu-like illness,or stomach infection. As the immune system fights off the infection, it mistakenly attacks the peripheral nerves.
The most commonly proposed mechanism for the development of autoimmune disease is molecular mimicry (Yuki, 2005). Molecular mimicry refers to the situation where the pathogen and host share nearly identical antigens, which induces an antibody and T cell immune response that is cross reactive.
N-9 of the nurses’ notes documents a PRECAUTION for a “resistant bacteria”, evidenced by a check mark in the upper right hand corner of that document, under the subheading for “INFECTION CONTROL PRECAUTIONS”. The same precaution is also noted in the upper right hand corner of the record at A-21. There are no further details.
At the time of her admission to the Kirkland and District Hospital, Arlene Berry’s blood pressure was documented at “115/70 bpm, with a pulse of 79 and regular”, with signs of “mild diffuse weakness” and “difficulty ambulating”, evidenced at A-6. The same record documents a "respiratory rate of 18", on admission. The normal adult respiration rate is 12 to 18 breaths per minute. At the time of this assessment, Arlene Berry was found to be “alert and oriented”, with “NO Focal deficits”. Notably, neurological examination in patients with Guillain Barre syndrome (GBS) may also reveal “no focal deficits”. A recent history of increasing or “diffuse muscle weakness” followed by paralysis suggests a typical presentation of GBS, especially if there was a recent illness, or infection, as in this case.
The emergency department record at A-6, what I take to be Dr. Spiller’s physical examination, documents a “soft, non-tender” abdomen, and “no masses”, suggestive of a typical admitting physical note to express an overall, normal, negative abdomen. A negative finding can also suggest hypotonia, a disorder that causes low muscle tone that results in muscle weakness. Hypotonia is often the presenting sign for many systemic diseases and diseases of the nervous system. The abdominal muscles feel ‘soft and doughy’; also a sign of gastropareses in clinical diabetes, which can rapidly progress to intestinal obstruction. Constipation is common due to hypotonic gut musculature. The lower limb is often ischemic in diabetes. Fecal impaction as a cause of acute lower limb ischemia is also reported in PubMed.
On examination, the physician who saw her documented positive “bowel sounds”, evidenced at A-6. Hyperactive “bowel sounds” provide the most immediate indication of persistent upper GI bleeding/GI hemorrhage. An accompanying crampy abdominal pain can also suggest acute bleeding. Fatigue, shortness of breath, lethargy and pallor may also be noted.
An increased white blood cell count may indicate an associated infection. Other findings may include hematemesis, coffee-ground vomitus, bloody stools (black or tarry stool), rectal passage of bright red clots and jellylike material (melena). Decreased urine output (urinary incontenence), tachycardia, and hypotension accompany blood loss; can also suggest shock from excessive blood loss.
Arlene Berry was still neurologically responsive when I saw her following her admission. She was able to reach and use for herself the kidney basin at her bedside table, as she occasioned to vomit more of the same flu-like “yellowish liquid” that she had done so many times on the days before, and in fact used it for herself in our presence, at which time a cool cloth was provided by the nurses, as evidenced by the record at N-6. The same record documents upwards of “100cc yellowish fluid”, what is frank bile, or ‘bilious vomit’ (toxic chemicals removed from the blood by the liver flow out of the body via the bile and digestive tract). The time of that assessment was documented at 1915 hours on May 23, 2000, following Arlene Berry’s hospital admission. The same record documents that the patient had stated she was “very tired”, whereupon she was then assisted to bed, as evidenced at N-6. In my opinion she was showing signs of progressive or perhaps even severe dehydration.
Vomiting is a symptom of many causes. Dehydration is the main concern with most vomiting. If the symptoms continue for days, they are usually considered severe. The clinical difference between bilious and non-bilious vomiting (ie, vomiting yellow or green) is critical in distinguishing life threatening abnormalities. The word “bilious” comes from the word cholera. The word cholera is Latin for bilious disease and has come to indicate a severe intestinal infection. People with bowel obstructions may repeatedly vomit yellow, or green colored bile and a history of frequent bilious vomiting in the presence of abdominal pain should have been a ‘red flag’ suggesting intestinal obstruction, which should have been treated emergently. Acute symptoms include bilious vomiting, diffuse abdominal pain, and bloody stool. Although stomach flu is by far the most common cause, intestinal obstruction is also the most serious and is considered a surgical emergency.
Arlene Berry also complained of being “cold” , she had the chills, and so the nurses provided her with extra blankets, evidenced at N-6. Her very last words were that she was at that time “feeling a little better”. Keep in mind that 12 hours or more of severe vomiting can make a person significantly dehydrated. The chills is just one of the signs and symptoms of severe dehydration.
For the record, symptoms of dehydration in order of severity are: thirst, nausea , chills, headache, fatigue, abdominal pain and dizziness. Other symptoms are increased heart rate, muscle pain, and reduced sweating. Dehydration can also potentiate constipation, concentrate the urine, and increase the irritative effects of dietary substances.
Iatrogenic hyponatremia?
Patients with clinically significant hyponatremia present with nonspecific symptoms attributable to cerebral edema. The symptoms of hyponatremia include: nausea and vomiting, restlessness and irritability, fatigue, slurred speech, and unsteady stride. Common symptoms usually include muscle weakness, lethargy, headache, and anorexia. These symptoms, especially when coupled with a recent history of vomiting resulting in altered fluid balance, should suggest the possibility of hyponatremia.
The presence and severity of symptoms are associated with the level of serum sodium, with the lowest levels of serum sodium associated with the more prominent and serious symptoms, which include decreased consciousness or coma. However, emerging data suggests that even mild hyponatremia (serum sodium levels at 131 mEq/L or above) has been associated with numerous complications and undiagnosed symptoms.
A-26 documents a body temperature >37.0 . According to that record the documented temperature is slightly above 37 C at approximately 37.8 suggesting a low-grade fever. Pathogenic bacteria grow best at human body temperatures in the 37 C range.
According to the medical record at N-6 Arlene Berry was admitted to the Kirkland and District Hospital at 18:45 hours and had spent 75 minutes in the ER, as evidenced at A-3. In all that time, the ED physician, Dr. Spiller had obviously done very little, as evidenced by the admission record, containing almost no information. NO simple blood tests were done or even ordered at that time. It is also clear that no course of action was charted, marked by a “routine” admission and a clinically evident inability on the part of the ED physician to adequately make a proper evaluation or to even make a provisional diagnosis. In fact, Dr. Spiller had no idea what was going on, or even what to look for, electing by reason thereof to play his feebleminded ‘wait-and-see’ game in the face of life threatening indicators.
The most common way in which doctors are negligent by failing to treat a medical condition is when they “dismiss” the presenting symptoms as temporary, minor, or otherwise not worthy of treatment. This situation may result in an exacerbation of the underlying condition or injury, causing further harm or injury. Emergency physicians have a primary obligation to treat emergency situations such as bowel obstruction.
Further, not only did the patient’s family physician fail to attend in a timely manner, NO diagnosis or differential was made following the patient’s admission at that time, or at all, according to record. Certainly, NO protocols were followed. Clearly, from the record as a whole, this patient was deliberately made to deteriorate.
A useful maxim to remember is “Not documented means not done”.
A-3 of the record, what I take to be the physician’s diagnostic chart is a “total blank”, like the physician whose name appears on it. Again, from that record it seems clear that nothing was entered because nothing was done. The same record was filed out-of-sequence. The emergency record at A-4 was also filed out-of-sequence. Interestingly both of these records were dated using a “rubber stamp” that is consistent with backdating techniques used by con artists.
The record at A-12, what I take to be physician orders documents a concomitant or concurrent administration of Senokot (laxative), MS Contin (narcotic analgesic), Statex (morphine family), and Gravol (an anticholingeric agent), including IV solution and additives, the most dangerous of which is the MS Contin, a brand name for Morphine Sulfate. Ms Contin has widespread effects in the central nervous system and on smooth muscle and produces respiratory depression by direct action on brainstem respiratory centers.
Co-administration of narcotic analgesics such as MS Contin with laxities, ie. Senokot may have additive central nervous system (CNS) and gastrointestinal (GI) system effects which can increase the risk of severe constipation or paralytic ileus, including CNS depression.
“Contin”, is a pharmaceutical industry buzzword for “time-release” or “continuous” release. Additionally, Arlene Berry had been given Statex, a narcotic: opioid agonist analgesic, also used to relieve pain, which also belongs to a class of the morphine family.
Morphine is contraindicated to sedation, brain tumors, or increased pressure in the head or spinal cord, possible abdominal problems requiring emergency surgery, and in patients having a substantially decreased respiratory reserve.
“MS” (morphine sulphate) is often confused with ‘Magnesium Sulphate’, used to treat severe constipation. Overuse of laxatives, or in combination with bi-phosphonates or magnesium sulfate, or an overdose of magnesium sulphate used to treat severe constipation can lead to hypermagnesemic pseudo-coma, which mimics a central brainstem herniation syndrome.
According to the record at A-13, Arlene Berry was given 30 mg (po bid) morphine by Nurse McCrank at 2000 hours on May 23rd, the eve of her death, in the face of an undiagnosed and undifferentiated condition(s) associated with “abdominal pain”. The administration of 30 mg MS Contin, like all opioid analgesics, can only serve to obscure the diagnosis or clinical course in patients with acute abdominal conditions. A judicious dose of morphine on standing order to patients with non-traumatic abdominal pain is usually in the range of 05. mg/kg. This patient was given 30 mg, a very significant difference.
The record at N-6 documents “telephone orders” received by the hospital from Dr. Jordan at 2030 hours for Stemetil 10mg by IV, x 4 daily for “control of nausea”, given by the RN, as further evidenced by the physician’s orders seen at A-11 of the record. Under normal circumstances, a typical single dose of Stemetil for a small woman with low body weight is 5mg.
Stemetil suppresses activity in the trigger zones of the vomiting center by “paralyzing the gastrointestinal tract” which "governs the vomiting reflex", which can also exacerbate dismotility.
The antiemetic action of Stemetil (prochlorperazine) may “mask the signs and symptoms of drug overdosage from other drugs and may obscure the diagnosis and treatment of other conditions”. Increased sedation is also a serious side effect of this type of agent.
Over-sedation results in obtundation, characterized primarily by reduced alertness and hypersomnia. Hypersomnia is defined as a state of sleep in excess of 25% of the expected normal.
Stemetil is widely distributed into body tissues and fluids. It undergoes metabolism in the gastric mucosa and on first pass through the liver where it enters the enterohepatic circulation and is excreted chiefly in the feces via the biliary tract. The drug falls in the same class of phenothiazines that have been known to suppress intestinal motility to the point of producing a paralytic ileus and precipitate or aggravate toxic megacolon, to add insult to injury.
Stemetil can also lead to changes in the blood-brain barrier (BBB), allowing an infectious agent to gain entry to the brain and produce lethal CNS ( central nervous system = brain and spinal cord) infection. The scientific literature describe two bacterial factors specific to the meningitis pathogen that thwart the normal protective role of the blood-brain barrier, leading to serious infection.
Blood borne infection in the blood lyse easily. It seems logical to assume that Stemetil would be contraindicated to serious infection for this reason.
Stemetil poisoning is marked by oversedation, respiratory depression and hypotension. Stemetil (prochlorperazine) intoxication or poisoning can also cause deep physiologic depression that resembles and can mimic brain death.
It is also clear that Dr. Jordan sought to eliminate the symptom “nausea”, without his attendance, as evidenced by the phone order “for control of nausea” and without any appropriate or timely blood-work, or addressing any possible underlying causes.
Further, Dr. Jordan neglected to consider the etiology of the nausea and vomiting as a condition requiring prompt medical intervention. Instead, he elected to give the patient a brain damaging antipsychotic-antiemetic neuroleptic drug without any review of her medical record, and without the benefit of diagnosis, toxicological screening or close monitoring, evidenced at A-21. Clearly, the etiology of the nausea and vomiting had never been considered, as evidenced at A-3.
Stemetil is a brand name for prochlorperazine. Morphine and prochlorperazine have a profound impact on bowel motility, often resulting in fecal impaction. The average adult carries about 15 pounds of dried fecal matter in the colon.
The co-administration of a narcotic analgesic (morphine) and a neuroleptic agent (prochlorpeazine) will result in neurolept-analgesia with drug-induced reduction of oxygen intake, resulting in respiratory depression.
Respiratory depression represents the principal negative variable introduced with “conscious sedation” and left unrecognized and untreated, is the cause of “panic”, including most serious complications.
Neurolept-analgesia, also called “conscious sedation” refers to the use of major tranquilizers, ie, prochlorperazine in conjunction with narcotics such as “morphine”. Neurolept-analgesia is defined as a state of CNS depression.
Notably, this patient had also been given penicillin-based medicines and sulfonamides such as Septra DS (Bactrim), and CIPRO (cyproflaxin) on the days before her admission; penicillin and sulfa-based antibiotics can cause the body’s immune system to react by over stimulation. Septra DS is an antibacterial agent with a wide spectrum of adversities (difficulty breathing; closing of the throat; swelling of the lips; and unusual bleeding).
Cross-reactions between penicillins and sulfa-drugs or sulfonamides are common triggers of drug-induced serum sickness and fixed drug eruptions.
Signs and symptoms of overdosage reported with sulfonamides include anorexia, colic, nausea, vomiting, dizziness, headache, fatigue, drowsiness, and decreased appetite. Hematuria may also be noted.
N-5 of the Nurses’ Notes documents “Sudden large queery bloody emesis, reddish brown liquid” at 0255 hours, on May 24th of 2000. Submit, when everything in the intestine slows down, everything in it usually backs up.
When the bowel is completely obstructed, the contents “back up” like in a kinked garden hose. This causes the tissue to become dilated with fluid and can impair the blood supply to the intestine, causing ischemia, or tissue death. Over time, the bowel then perforates, or ruptures, causing the spillage of harmful bowel contents into the abdomen. Gastrointestinal bleeding ALWAYS requires prompt physician evaluation and intervention.
When the bowel wall is ruptured, this unsterile material contaminates the abdomen and the organs with which it comes into contact. This is extremely dangerous to a patient, as it quickly causes an inflammatory reaction called peritonitis and can lead to a system-wide infection called sepsis.
N-3 documents an “Suctioned orally thick brownish secretions” at 0320 hours (in the small hours of the morning), suggestive of a more significant backup of intestinal material, ie., vomiting of "fecal matter" due to obstruction of the bowel, evidenced by family present as a large “chocolate colored (gross appearance), odorless, pasty material, looking pretty much like feces". If you are unable to open your bowels due to an obstruction somewhere, then your feces cannot exit your body via the normal route and you can get nauseated and start to vomit fecal matter. This condition requires urgent medical attention and probably surgery.
The same record documents “suctioned down ET tube several times for small amount of brownish mucous” (a reddish brown liquid, suggestive of old blood or admixture of blood and gastric content) at 0330 hours, while A-17 documents “being suctioned for moderate amounts of coffee-ground emesis by RN” at the very same time on May 24th.
Suctioning infers that the patient’s airway has become obstructed with secretions or debris. Any negligence of the patient’s throat secretions may lead to hypoxia, brain edema and further deterioration in a patient’s condition leading to a vicious circle, which if not broken will lead to death.
For the record, the inability to adequately clear secretions associated with respiratory muscle weakness is a common finding in both GBS and WNV encephalitis.
West Nile virus (WNV) can cause severe, potentially fatal neurological illnesses, which include encephalitis, meningitis, and Guillain Barre syndrome.
WNV season: May through October. A person with WNV-associated acute flaccid paralysis may present with or without fever or mental status changes, although fever is more common.
The record at A-5 documents a blood pressure of 115/75 at 17:05 hours on May 23rd that by 18:45 hours had dropped to 100/50 bpm. Marked blood pressure lability with alterations between hypertension and hypotension following paresis suggests an atypical course of Guillain Barre syndrome.
A-20 of the record documents a Glucose of 13.2 H mmol/L (the normal range is 4.1 – 7.8). High blood sugar usually comes on slowly. To convert mmol/l of glucose to mg/dl, multiply by 18. (13.2 x 18) = 237.6 mg/dl.
Random Blood Sugar Test (RBS) measures the level of glucose in the body at any point of time. If the level of sugar is between 140 mg/dL and 200 mg/dL, the patient is diagnosed with pre-diabetes. If the level of sugar exceeds 200 mg/dL, then the patient is diagnosed with diabetes.
Glucose levels of 11.1 mmol/l (200 mg/dl) at 2 hours confirms a diagnosis of diabetes. Symptoms of severe high blood sugar (hyperglycemia) include drowsiness and difficulty waking up. Further, phenothiazines, such as the drug Stemetil, have even been reported to trigger diabetes in patients with no previous history of diabetes. Other causes include Panic (pan-ik), or the phenomenon known as "scared stiff".
A sudden overwhelming fright =adrenaline. If you become exhausted, stretched thin, with a body reeling from too much adrenaline, sugar – chances are that your deeper brain will soon succumb to sensory overload resulting in alterations in body chemistry. Absolute fright and the consequent “shock” will “shut down” one’s cognitive abilities just as surely as sensory overload will jam the survival circuits of any living organism. The most common reaction: “paralysis” due to total sensory overload.
sensory overload
hyperventilation, pounding heart (tachacardia), misinterpretation, fear
arousal —> dizziness —> e.g., “I’m dying” —> panic –
^ |
adrenaline* breathlessness | | symptoms <- normal body changes etc.
Adrenaline*raises the blood sugar glucose level.
A-19 of the record documents an elevated WBC Count of 22.4 H. WBC = Leukocytes, the White Blood Cells. The presence of an elevated WBC count is called Leukocytosis. White blood cell count is actually 22,400. A normal WBC is 5,000 to 10,000. Normal Adult Range: 3.8-10.8 thous/mcl. Optimal Adult Reading: 7.3.
An increase in WBCs may occur in many conditions, including infection (viral, bacterial, fungal, and parasitic), allergy, leukemia, hemorrhage, traumatic tap, encephalitis, and Guillain-Barre syndrome. The WBC differential helps to distinguish many of these causes. For example, viral infection is usually associated with an increase in lymphocytes, while bacterial and fungal infections are associated with an increase in polymorphonuclear leukocytes (neutrophils).
WBC’s are the body’s primary defense against bacterial infection and also reflect the degree of physiologic stress. WBC’s are also elevated with dehydration, and hyperviscosity secondary to dehydration. A high WBC may also indicate that there is inflammation of the central nervous system, as in meningitis, for example.
If the total WBC is high due to a rise in neutrophils and eosinophils, then an allergic, or parasitic process is most likely. Other causes of an increased neutrophil count include cerebral abscess, following seizures and following CNS hemorrhage. An increase in the WBC count (leukocytosis) is also a typical response to noxious stimuli.
The record at A-19 documents a Neutrophil count of 92.0 H with an absolute neuts of 20.0 H. Neutrophilia (or neutrophil leukocytosis) is a condition where a person has a high number of neutrophil granulocytes in their blood.
Cerebrospinal fluid pleocytosis with neutrophil leukocytes in Guillain-Barre syndrome is reported in the European Journal of Neurology. 11(9):645-646, September 2004.
Neutrophils, are also known as “segs”,”PMNs” or “polys”(polymorphonuclears). PMN are the primary effector cells in the innate immune response against infection.
CSF in bacterial meningitis is typically dominated by the presence of PMN’s. PMN’s generally predominate in bacterial infections. Neutrophils are associated significantly with the density of parasites, such as amebiasis.
Notably, cancer-suppressing protein is part of ameba’s compass.
Polymorphonuclear leukocytes accumulates in brain regions with low blood flow during the early postischemic period.
Neutrophilia may also be due to a number of acute and chronic causes such as infection, inflammation, emotional stimuli, drugs, metabolic hormonal, and endocrine disturbances, including hematologic abnormalities. The presence of polymorphonuclear granulocytes does not rule out the diagnosis of Guillain-Barre syndrome. Eur J Neurol 10(5): 479-86. Occasionally, polymorphonuclear leukocytes are seen in severe cases. Macrophages then infiltrate and migrate to the myelin sheath, eventually causing the destruction of myelin sheaths.
Leukocytosis, especially neutrophilia, indicates systemic infection and is rare in the absence of bacterial “superinfection”, also called “superbugs”, such as bacteria, viruses or mixed infections which are resistant to antibiotics.
Wegener’s granulomatosis, granulomatous cerebral amebiasis, vasculitis, and heart attack are high on the order of Neutrophilia.
The record at A-19 documents a Lymphocyte count of 2.0 L (low) suggestive of lymphocytopenia in which lymphocytes (T-cells) are reduced with nutritional deficiency, infection, and ascites due to “fluid build-up in the abdomen”, including an exhausted immune system. If bacterial infection is present in ascites this may suggest spontaneous bacterial peritonitis, in which abdominal pain is a prominent finding. If peritonitis is not treated promptly and effectively multisystem organ failure occurs rapidly.
A-19 documents a Red Blood Cell (RBC) count of 4.30 (3.80 – 5.80 is normal), but the HCT Hematocrit (HCT) is very low, with a reduction suggestive of anemia. Know that red blood cells placed in a hypotonic solution (e.g., pure water) burst immediately (“hemolysis”) from the influx of water. Because red blood cells are being destroyed, the person quickly becomes anemic and pale. The result is a lot fewer red blood cells to carry oxygen.
The same record seen at A-19 documents an HCT (Hematocrit) count of only 0.361 L (low): HCT is the measurement of the percentage of red blood cells (RBC’s) in whole blood. The hematocrit (HCT) is another way of measuring the true amount of hemoglobin (Hb), and in this case it is very low. Thus anemia is present when HCT is < 1.0 x 109/L.
A-19 documents a Monocyte count of 3.0. The monocytes are a type of phagocyte which mature into “macrophages”; they are important germ eating cells. Patients with a low monocyte count have a higher risk of getting sick from an infection, particularly those caused by bacteria. In this case the Monocyte count is in the low normal range.
The majority of patients with Guillain-Barre syndrome will have 10 or fewer monocytes. In cancer, or leukemia, the monocytes become elevated.
A-20 documents the O2SAT (oxygen saturation) with an arterial oxygen saturation (SaO2) of 98.9 H, with a NORMAL reference. The same record documents an Arterial pH of 7.437. The ideal pH for blood is 7.4. The time of that assessment is documented at 0400 hours on May 34th of 2000, only 8 hours before she was pronounced as having met with brain death criteria.
Hydrogen ion concentration expressed as pH “Power of Hydrogen” (Humans as organisms) scale of acidity/alkalinity. pH below 7 = acidic, pH above 7 = alkaline. Neutral pH is 7. Acids and alkalis are the chemicals at each end of the pH spectrum. The scale runs from 0 (acid) to 14 (alkali). For example, the pH of blood is normally 7.4 and that of muscle is 7.0. pH under 7 is acid; pH over 7 is basic or alkaline. The metabolic pathways of the body require a slightly alkaline environment. Ph 7.0 and higher indicates alkalinity. A Normal pH is 7.35 – 7.45. When blood is a pH of 7.43 – only slightly alkaline – optimal.
Our blood pH has a very narrow range of around 7.35 to 7.45. If our body’s pH deviates from this range, we will be sick or have symptoms of falling sick. a blood with a pH value of 7.45 contains 64.9% more oxygen than blood with a pH value of 7.30. The heart is normal when the pH of blood plasma is slightly alkaline, having a pH of 7.35 to 7.41. An absolute blood measurement of acidity (pH below 7.0) is incompatible with sustaining life. It is a known fact that cancer thrives in an acidic (pH) environment in the body, but cannot survive in an alkaline (pH) environment. At a pH slightly > 7.4 cancer cells become dormant.
With metastases the pH drops to 6.0 and even 5.7 or lower. Terminal cancer patients are around 1000 times more acidic than normal healthy people. The vast majority of terminal cancer patients possess a very low body pH. In this case, pH – optimal is as good as it gets.
A-18 of the medical record documents an “inferior ischemia”, a sign of reduced oxygen supply to vital organs due to reduced or poor blood flow to the heart. Inferior ischemia means that a portion of your heart (lower) muscle is not getting enough blood supply. It usually occurs as a result of a blockage in one of the arteries supplying that portion of the heart muscle with oxygen.
Inferior ischemia is decreased blood flow to part of the heart (the inferior part). This is a serious condition, and can be predictive of what is commonly known as a “heart attack”. An inferior ischemia is the hallmark of “impaired organ perfusion”, as it implies that, unless corrected, there may not be enough oxygen in the blood to sustain vital organs.
In GBS individuals, deep venous thrombosis or thromboembolism is very well known; due to the formation of a blood clot(s); occurs in arteries that supply the heart.
The same record at A-18 documents “Sinus Tachycardia”. Sinus tachycardia occurs when the sinus rhythm is faster than 100 beats per minute. Sinus tachycardia, (>90/min), is seen in over 35% of patients with Guillain-Barre Syndrome, and over 30% suffer from hypertension (Parry, 1993).
A-20 documents a Sodium level of 144. The reference range for normal is 137 – 145 mmo1/L. Sodium is an electrolyte that helps with nerve and muscle function, and also helps to maintain blood pressure. Sodium circulates in the body fluids outside the cells. It is very important for maintaining blood pressure. Sodium is also needed for nerves and muscles to work properly. CAVEAT: Serum Sodium is lowered 1.6meq/L for every 100mg/dl glucose should be borne in mind..
A-20 also documents a Serum Potassium level of 3.4 L at 0400 hours on May 24th of 2000. Hypokalemia is defined as a potassium level below 3.5 mEq/L. Further, during episodes of hypokalemic periodic paralysis associated with a low potassium level, urinary output is decreased during the attack because water accumulates intracellularly in muscles.
The same record documents a Sodium level of 144 mmo1/L. The normal reference range is 137 – 145. High sodium levels are usually a symptom of dehydration with a reduction in this case, attributed to increases in glucose. Know that hyperglycemia can lower the serum sodium concentration by 1.6 mEq/L for each 100 mg/dl as the high levels of glucose draws intracellular water from overzealous IV infusion into the extracellular space, giving rise to a false test.
There is undoubtedly an involvement of metabolic derangement and neuronal injury in the detrimental effects of hyperglycemia. Hyperglycemia is particularly detrimental in ischemia/reperfusion. Hyperglycemia is also reported to trigger massive neutrophil deposition in brain following transient ischemia. If tissue invasion is mild, small areas of necrotic tissue resorption may occur, but if the bacterial invasion is massive, acute suppurative abscesses can arise.
The same record seen at A-20 documents a CK (creatine kinase) level of only 40 units per liter (U/L) at 0400 hours. In females, total Creatine Kinase should be 10-79 units per liter (U/L). The creatine kinase level usually parallels a disease activity. In normal conditions, there is very little Creatine Kinase circulating in the blood of the average, healthy human being. Know that CK is the most sensitive enzyme and in the presence of most diseases, levels can be elevated as much as 50 to 100 times the reference level. The hallmark of muscle wasting (or muscle damage) is elevation of CK. The wasting away of fat and muscle (cachexia), is the most visible hallmark of metastatic cancer. Persons with cancer typically have high CK levels.
Elevation of CK may also be seen in stroke, extreme shock, and brain tumors in which CK levels can sometimes temporarily go off the scale, topping out at 50,000 to 200,000 U/L, a sign of severe muscle fiber breakdown (necrosis). CK levels may rise significantly in about 2 to 3 hours. Taking a good history is important in these circumstances. Significant increases in serum CK have been observed and reported in cases of adenocarcinoma and SCAC of the lung with proven CNS metastases, while patients with oncological conditions other than SCAC of the lung have failed to show elevation in serum CK.
In this case, CK is well within the normal range. Serum CK is considered a useful diagnostic marker or indicator of active metastases, while patients with oncological conditions have "failed to show elevation in serum CK".
Elevation of CK is not an acute finding in Guillain-Barre syndrome.
EVIDENCE OF SUBSTANDARD CARE
N-10 of the Nurses’ Notes document the patient’s level of care as “routine”, which showed little or NO concern for patient safety in the face of life threatening indicators.. Further, NO close patient monitoring or toxicological screening was done, marked by a complete absence of nursing care plan, as evidenced at A-21 of the medical record. In fact, NO inherent bloodwork was done in a timely manner. NO protocols were ever followed or implemented, in this case.
The record at 0020 hours seen at N-6 documents the discovery by duty nurses of the patient’s “head against the left side bed rail with her feet under the right side rail” suggestive of sensory loss. Sensory loss in Guillain Barre syndrome, if present, takes the form of proprioception, or “loss of sense of one’s own perception of the relative position of neighboring parts of the body to each other”, which is occasionally impaired spontaneously, especially with extreme fatigue.
The ED physician, Dr. Mark Spiller was up to assess the patient’s condition. Upon examination the patient's eyes were documented as being “sluggish”. She was simply repositioned by the nurses, as evidenced by the record at N-6. Her “pupils were dilated at approx. 5 mm” with “very little reaction to light”, and far from getting better she was becoming progressively worse, as evidenced by a sense of urgency seen on the record to the attendance of the patient with increased activity evidenced at N-6 between 0030 and 0055 hours, also noted at N-5.
Clearly, from that record and apart from running around the room looking busy and repositioning the patient, nothing was done. It seems clear that the ED physician failed to properly assess the patient’s condition, which fell far below an acceptable standard of care. Further, to add insult to injury, NO blood-work had yet been done.
While the clinical feature of ‘fixed dilated pupils’ is a valuable clinical sign it does not necessarily mean that the patient has severe brain injury.
I assume that Dr. Jordan would have been alerted by phone. He claims to have called in at 0100 hours but nevertheless opted not to change his orders, as evidenced by the “no change in orders” seen at N-5. From that record it is clear that Dr. Jordan elected to alienate and treat the patient over the telephone, unseen, in the face of life threatening indicators, all of them ignored and without ever having reviewed the patient's record.
Further, between 0200 hours and 0220 hours the patient’s blood pressure had risen slightly from 150/72to 162/80, a sign of mounting hypertension such as caused or worsened in response to treatment. The record at A-26 documents the time of that assessment as 0220 hours, while N-5 documents the time of the same assessment at 0230 hours, a 10 minute difference. The same record documents a HR (heart rate) in the 160′s, what is termed “sinus tachycardia”.
A-26 documents a blood pressure of 162/80 with an SaO2 of 80% at 0220 hours, followed by a lethal drop in blood pressure to 78/70 by 0235 hours, in which blood pressure rises or falls significantly, a hallmark feature of alternating hypotension and hypertension.
CAVEAT: Systolic blood pressure <80 mm HG is a hallmark of haemodynamic instability. The term “hemodynamic instability” is most commonly associated with an abnormal or unstable blood pressure, especially hypotension, or trauma due to clinical insult. Hemodynamic instability has also been defined more broadly as global or regional perfusion that is not adequate to support normal organ function. This definition recognizes the obligation to insure adequate organ perfusion during the flaccid period in patients with GBS.
The record at A-17 documents a complete cessation of the use of abdominal and accessory muscles, evidenced by a “0 use of acc muscles”; and a “0 use of abd muscles”; the muscles of respiration, accessory muscles and diaphragm are affected, suggestive of respiratory and accessory muscle paralysis (crisis) requiring intubation and mechanical ventilation. Functional abdominal muscles also play a role of in conjunction with the accessory expiratory muscles. The time of that assessement is documented at 0330 hours. Accessory muscle paralysis results in apprehension and anxiety.
EVIDENCE OF ALTERED RECORDS
There are numerous material deficiencies in the related medical record of Arlene Berry which manifest a complete lack of internal consistency, ranging from out of sequence records, from the physician’s Discharge note seen at A-1 and A-2, which is marred by error, inconsistency, omission, and contradiction, to the nurses Triage, to obviously rewritten, altered, and/or falsified portions of the medical record, obviously tailored or larded to obfuscate the truth, seen between N-1and N-3 of the nurses notes, with A-16 and A-17 presenting similarly, including as follows:
A-26 of the record documents a BP (blood pressure) of 78/70 at 0235 hours, while N-5 documents a BP of 98/70 at the very same time, suggestive of copious error.
A-4 of the record, what I take to be a Trauma Legend, barely visible in the physician’s notes situated in the lower right hand side of that record, there is an obliterated area suggesting a white-out, or perhaps an erasure. From that record it seems clear that relevant information was deliberately withheld, or removed to conceal an event.
TRAUMA is defined as any insult to the body, clinical or otherwise. Notably, A-24 documents a heart rate of 174 bpm at 0320 hours that is consistent with trauma.
The record at A-6 documents a “history of metastatic lung cancer”, while the outpatient record at OP-54 clearly documents “no metastasis” and “mediastinoscopy negative”.
N-4 presents with less than half a page of documentation consistent with deliberate omission, such as having rewritten that record for the express purpose of withholding incriminating information.
A-16 documents a blood pressure of 163/117 at 0330 hours while N-3 documents a blood pressure of 136/85 at the very same time. The same record documents a blood pressure of 121/81 at 0400 hours, while N-2 documents a blood pressure of 112/57 at the very same time that is consistent with more copious error.
N-4 of the record documents that Dr. Jordan was called in at 0225 hours. A-1 of the record documents “I was called in later that night because the patient had become obtunded”, while the record at N-2 documents “attempts to pull away to painful stimuli” as late as 0400 hours on May 24th, being one hour and thirty-five minutes later, according to that record. In coma, a person is highly unlikely be roused to painful stimulation.
Was it the doctor’s belief that Arlene Berry ceased to be a human being after becoming unresponsive following undiagnosed, untreated and/or inappropriately treated conditions? So much so that he decided to write her off? Or was there a more sinister plot afoot? Such as procurement of her eyes?
N-10 of the record with respect to the patient’s bowel routine and urinary elimination pattern for toileting is a complete blank, with the very same information that ought to have been recorded, also omitted at OP-53 of the record, also suggestive of neglect.
The record at N-5 documents a physician “assessments unchanged” at 0235 hours despite the fact that the patient had already gone into respiratory distress at that time, as evidenced by “Cheyne-Stokes” respirations with periods of “apnea” lasting “5-8 seconds”. Sleep apnea means cessation of breath. It is characterized by repetitive episodes of upper airway obstruction that occur during sleep, usually associated with a reduction in blood oxygen saturation. Other causes include panic attacks.
Low oxygen saturation may be present with advanced respiratory muscle involvement. If proper balance is not promptly restored or corrected, the heart and lungs may fail and the brain will literally begin to suffocate.
The record at N-5 documents the respirations as “deep and soaring without constant jaw lift”as early as 0220 hours. A-26 of the record documents “gurgling”, and “snoring” and is evidenced in the lower left corner of that record.
N-5 of the record documents “family in” at 0250 hours. On seeing the patient, we found her to be propped up in the arms of two nurses, gasping for air, with only a plastic oral airway in her mouth. A reason for this , according to the duty nurse was “to keep the patient from swallowing her tongue”. Weakness of tongue and retropharyngeal muscles causes positional airway obstruction; difficulty with protruding tongue and difficulty swallowing indicate that bulbar involvement is significant. Snoring, sleep apnea and gasping for breath are part of the same problem.
Noise heard during any part of the respiratory cycle may indicate airway obstruction or alteration in airway patency.
Patients with neuromuscular disorders have rapid, shallow breathing secondary to severe muscle weakness, which requires that these patients be placed on ventilators in order to breathe. Failure to manage the airway with endotracheal intubation when necessary or in a timely manner is clear evidence of negligence.
I had asked the patient twice, in the presence of her foster brother, if she could hear me to wiggle her toes, and indeed she did, not once but twice, to be absolutely certain. An observation made by her foster brother as he gently stroked her right cheek was the seeming appearance of the patient attempting to pull her face forward as though trying to lift her head off the pillow. The inability to lift the head off the pillow by flexing the neck is another danger sign associated with GBS; it frequently develops simultaneously with phrenic nerve (diaphram) weakness.
In my opinion, Arlene Berry appeared to be more paralyzed or blunted than anything, with the exception of lower limb joint contractions which rapidly diminished and became hyporeflexic.
Her condition on the night before her death was cataleptic-like, characterized by a profound hypnotic state, or psychomotor condition of morbid sleep, such as seen in cataplexy, neurolepsis, sleep paralysis, or narcolepsy. Underlying causes of catalepsy include severe emotional trauma, and emotional shock. Compare: neuroleptanalgesia (conscious sedation) in combination with a severely paralyzed motor function.
Although patients with GBS in the setting of preserved consciousness may appear to be completely obtunded, they are technically awake and fully lucid. But he/she may literally not be able to move a muscle in response. The GBS patient only appears to be unresponsive due to a severely paralyzed motor function. It has been shown that more than half of the time it is the family and not the physician who first realized that the patient was aware.
Stupor and coma are characterized by impairment of the arousal system. In stupor, a person arouses only in response to strong verbalor tactile stimuli, awakens briefly, and then lapses back into a sleep-like state after the stimulation stops. In coma, a person cannot be roused to consciousness.
With GBS the patient is conscious but unable to respond due to a severely paralyzed motor function.
N-3 of the record documents “resp noisy”,”shallow”, “Cheyne-stoke” at 0320 hours. Cheyne-stokes breathing is a respiratory pattern that oscillates between hypoventilation and hyperventilation, usually the result of diencephalic insult. It may also be seen during sleep in some normal individuals.
For the record, hypoventilation and hyperventilation is commonly seen in patients with GBS. Hyperventilation = too much gasHypoventilation = not enough gas exchange. exchange.
N-5 documents a “sudden large bloody-emesis of reddish brown” at 0255 hours , what is known in medical circles as “coffee-ground emesis” ie. dark brown tinged vomit the color and consistency of coffee-grounds, composed of gastric juices and old blood, which can rapidly grow bacteria. Vomit that contains blood may have a red or brownish red appearance and is called coffee ground emesis, indicating that it has come from large intestines, suggestive of a slow bleeding source in the upper GI tract. Obstruction below the middle of the small bowel also gives rise to brownish vomit.
Gastrointestinal (GI) bleeding due to stress ulceration in GBS is reported in the literature. GI bleeding is considered a potential medical emergency. It involves assessing hemodynamic stability, resuscitating the patient as needed, locating the source of the bleed, and treating the underlying cause. From the record it seems clean that NO emergency measures were taken with respect to GI bleeding and that this medical EMERGENCY event was met by the doctors with complete indifference.
The record at N-4 documents “incontinent blood tinged urine”at 0305 hours. Incontinent “tinged urine” is consistent with severe dehydration, often mistaken for hematuria (blood in urine). Incontinence can also be the result of hypotonia, or neurogenic bladder.
Know that severe forms of GBS may result in urinary or fecal incontinence. A history of grossly bloody stools may be observed; fecal leukocytes are usually present.
N-3 of the record documents a “large amount of dilute urine” (polyuria) at 0325 hours, only 20 minutes later. This finding is inconsistent with hematuria, but may suggest diabetes insipidus, or a patient demonstrated hypotonic hyponatremia with maximally dilute urine consistent with IV overload. Because of the excretion of abnormally large volumes of dilute urine, you may quickly become dehydrated. Also know that the color and volume of urine can be a reliable indicators of hydration level. The output of a large volume of dilute urine leads to extracellular dehydration.
A common cause of hyponatraemia is hypotonic dehydration and iatrogenic water overload (eg overestimation of the degree of hydration, inappropriate use of hypotonic solutions for rehydration and/or too rapid administration of maintenance fluids). Other causes include the syndrome of inappropriate antidiuretic hormone hypersecretion (SIADH), especially in patients with meningitis. SIADH is a volume-expanded state due to ADH-mediated renal water retention.
In this case, the patient demonstrated hypotonic hyponatremia with maximally dilute urine is consistent with water intoxication. SIADH is water overload and not salt depletion. This leads to excess water elimination as dilute urine.
The record at N-2 documents “Foley draining lge amt dilute urine” again at 0425 hours, while N-1 of the record documents “Foley catheter emptied for 1200cc dilute urine” at 0450 hours that is consistent with conditions featuring osmotic diuresis, such as diabetes insipidus or “water diabetes”. It occurs in association with Na+ Disorders, primarily related to Na negligence, due to iatrogenic fluid overload.
The central causative mechanism in this case, involves an untreated hyperglycemia-induced osmotic diuresis and resultant dehydration. Polyuria due to excess fluid intake and glucose-induced osmotic diuresis is common in patients with transient hyperglycemia. The hyperglycemia emanates from a commonly identified diabetogenic stressor, such as infection, which precipitates the onset of the syndrome, which in turn produces pseudohyponatremia commonly associated with hyperglycemia. Another is drug-induced hyperglycemia, which should not be overlooked in this case.
Polyuria has been observed in a severe case of GBS. Polyuria in GBS is multifactorial and would be partly due to a dysregulation of osmoreceptors. Besides dangerous cardiac manifestations, neuro-endocrine changes are also reported and could induce electrolytes and fluid balance impairments.
A-15 documents the 24 hour IV fluid balance record, that between 1745 hours and 0200 hours was administered as follows:
A-14 documents an ” IV gid prn”, meaning that fluid and medication rate of administration to be is given by IV as follows: 3.3 % dextrose (a sugar solution used in intravenous drips) and 0.3 % sodium chloride solution (referred to herein as “2/3 and 1/3″) at the rate of 100 cc/hr, together with the medications, as evidenced at A-15.
The combination of 3.3% dextrose and 0.3% sodium chloride (known as 2/3 and 1/3) contains only 51 mmol/L of sodium. Outside of the body, the osmolarity of the solution is 269 mOsmol/L (sodium and dextrose combined). Once the solution is infused, however, the dextrose is rapidly metabolized, which leaves two-thirds of the solution (667mL) as electrolyte-free water and renders the solution extremely hypotonic.
CAVEAT: A red blood cell placed in a hypotonic solution (ie, pure water) bursts immediately (“hemolysis”) from the influx of water. Other conditions that can cause hemolysis include immune reactions, toxins and poisons.
The patient will suffer a decrease in the osmotic concentration of the plasma which is now hypo-osmolar to red blood cells and so water enters freely by osmosis and the cells swell and eventually burst, resulting in lysis of many red blood cells and the inability to oxygenate the brain, etc., and the patient is made to further deteriorate.
Hypotonic dehydration causes the amount of deficit to be overestimated by physical examination. It is important to note that hyponatremia more often represents excess of water than insufficiency of sodium.
Further, it is never appropriate to use the combination of 3.3% dextrose and 0.3% sodium chloride (known as 2/3 and 1/3) as “initial” fluid resuscitation in the dehydrated patient. Its use is limited to those who have severe hyponatremia unresponsive to isotonic saline boluses or who need concomitant fluid restriction.
To restrict fluid resuscitation and/or subject a patient to overzealous water overload, especially in an already in an already severely dehydrated patient is outright stupidity, and constitutes an act of wanton and reckless disregard for human life. Adequate sodium balance is necessary for transmitting nerve impulses and proper muscle function, and even a slight depletion of this concentration can cause problems.
If there is reason to be concerned about impaired function of the brain, heart, or kidneys, it is always prudent to rehydrate more slowly. This empirically-derived approach minimizes the cerebral disturbances (e.g., seizures, cerebral edema) caused by fluid shifts that can occur if fluid is infused too rapidly. It needs to be clear that all guidelines regarding fluids and electrolytes are approximations that in no way can replace careful monitoring of the patient, which was not done in this case.
The record at A-15 documents a total IV solution + additives of 1000 cc TBA, (to be absorbed), documented by Nurse Bates at 1745 hours; with a 150 ABS (absorbed) by 1900 hours, documented by Nurse Ferguson, shows 150 cc absorbed over a period of 75 minutes; exceeds the rate of 100 cc/hr by 25%. Anything above the 100 cc/hr points to “overly rapid infusion” leading to overhydration or “water intoxication”, which mimics features of diabetes.
Solution + Additives of 850 cc TBA remaining at 1900 hours documented as ABS (absorbed) by 0200 hours, over a period of 7 hours, resulting in a “surplus” of 150 cc fluid, with an additional 1000 cc TBA, and NO further documentation with respect to IV monitoring. The record shows a complete absence of information with respect to “Water Refill”, suggestive of NO close monitoring, or possible IV withdrawal after overload.
Hyponatremia results from a “surplus of water” due to negligence. Other evidence of fluid overload as indicated by “ascites” due to fluid build-up in the abdomen, marked by lymphocytopenia, evidenced at A-19.
Irreparable harm can befall the patient when abnormal serum sodium levels are corrected too quickly or too slowly. Rapid correction of hyponatremia, even mild hyponatremia, risks neurologic complications (see Fluid and Electrolyte Metabolism: Osmotic demyelination syndrome). Generally, Na should be corrected no faster than 0.5 mEq/L/h. Increase should not exceed 10 mEq/L over the first 24 h. Any identified cause of hyponatremia is usually treated concurrently.
Hyponatremia may occur in up to one-third of patients with Guillain-Barre syndrome and the syndrome of inappropriate antidiuretic hormone (SIADH) has been reported to accompany the neurologic manifestations of the Guillain-Barre syndrome. An association between SIADH and diabetes mellitus has also been reported; the basic fluid problem in SIADH is water overload and not salt depletion. One of the most potent stimuli for ADH release is nausea and vomiting.
Use of hypotonic fluids in presence of circulating ADH can causes free water retention resulting in hyponatremia. Other nonosmotic stimuli for the release of ADH include pain, stress, fear gastroenteritis, hypoxia, positive pressure ventilation, trauma, and medications such as opioids. Hyponatremia exerts most of its clinical effects on the brain. Brain volume is regulated by equal osmolality of extracellular and intracellular fluid. When extracellular osmolality decreases, water influx occurs in the brain resulting in cerebral edema due to electrolyte-free water moving into the brain cells. Cerebral edema is responsible for symptoms such as headache, nausea, vomiting, irritability, and seizures.
The record at N-6 documents “IV infusing well”, suggestive of overzealous IV infusion. Be aware that rapid administration of hypotonic IV fluids can cause swelling of the brain cells, and increased intracranial pressure. Further, rapid correction of hyponatremia may result in brain dehydration, cerebral bleeding, demyelination, neurologic injury, or even death. The same record documents a “hard” IV site in the “R” (right) hand; clot formation due to irritation, of the vein from solution or medications is the most common cause of a hard IV site. The back of the hand has weaker veins.
Correction of serum sodium that is too rapid can precipitate severe neurologic complications as a result of intracerebral osmotic fluid shifts and brain edema. This neurologic symptom complex can lead to tentorial herniation with subsequent brain stem compression and respiratory arrest, resulting in death in the most severe cases, the primary cause of morbidity and death is brainstem herniation and mechanical compression of vital midbrain structures.
Seriously ill patients always require accurate fluid balance monitoring because IV fluid also contains the medication(s). Rapid infusion may also lead to over-dosage. There are no further IV related entries on the record, either to indicate when or if the IV was discontinued, or to show that the rate of administration was being accurately monitored, or modified, suggestive of deliberate omission, or iatrogenic neglect.
CAVEAT: Remember, water follows sugar (and salt). If all the sugar is in the blood, not the cells, then the patient is dehydrated. Further, sugar solution in IV creates gaps in the blood-brain barrier allowing chemicals to enter. Infected material can block the blood vessels to the brain, and drugs such as Stemetil can help shuttle it directly into the brain and CNS. Once across the blood-brain barrier, the infection enters neural cells, with resultant disruption in cell functioning, perivascular congestion, hemorrhage, and inflammatory response diffusely affecting gray matter disproportionately to white matter.
Circulatory overload can occur if IV is not regulated properly and IV fluids infuse too rapidly for the patient’s body to handle. Signs of fluid overload include tachycardia, elevated blood pressure, dyspnea and other signs of respiratory distress. Neuromuscular disease is another well-known cause of dyspnea.
Notably, Stemetil 10mg was added to the IV at 2030 hours. The drug is sedating and a potent vasodilator, which also crosses the blood-brain barrier. Patients are usually “volume expanded” prior to its use, resulting in neurologic derangement. This is no coincidence. Hospitals are on constant watch for organs, and are known to provoke fatal outcomes in cases where they are likely to obtain body parts.
Hyponatremia is diagnosed by measuring serum electrolytes. It should be noted that hyponatremia occurs not because of loss of sodium but because of gain of free water. However, serum Na may be artifactually low when severe hyperglycemia increases osmolality. Water moves out of cells into the ECF. Serum Na concentration falls about 1.6 mEq/L for every 100-mg/dL (5.55-mmol/L) rise in the plasma glucose level above normal. This condition is called translational hyponatremia because no net change in the amount of Na has occurred.
The record at N-4 documents the patient’s “transfer to ICU in respiratory distress” at 0320 hours, while record at N-3 documents a “congested oral airway” at the very same time, meaning congestion of the breathing passages. Obstruction of the air passages of the nose, mouth, or throat may also lead to difficulty breathing. Certainly the inability to breathe properly can be alarming, and many persons will immediately react with anxiety, fear, or panic.
The record at A-24 documents the mechanical charting of the patient’s vital signs that commenced recording at 0315 hours. It is interesting to note from the the paper record that the patient’s transfer to the ICU had not yet taken place, and that no prior attempt was made by any of the health-care providers to place the patient in the ICU prior to 0320 hours. It seems clear that the health-care provider had done too little too late, as evidenced by the records at N-9, N-10, N-11, including A-3, and A-21.
From the record as a whole, it is also clear that both doctors should have realized at the onset, from the severity of the patient’s signs and symptoms that they were faced with a critically ill young woman who was not responding to their questionable treatment. They should ALSO have been acutely aware of the danger. Critically ill patients frequently have multiple physiologic derangements that come from a range of possible sources and they usually occur simultaneously.
N-5 of the medical record documents a gurgly respirations as evidenced by a “gurgly resps” at 0220 hours, a sign of constriction suggestive of thoracic trauma (patients are often in shock). The same record documents “deep and soaring and without constant jaw thrust”, such as associated with the airway and swallowing difficulty in respiratory compromise. Gurgling is a bubbling sound. It usually indicates upper airway obstruction from secretions. Gurgling respirations indicate the presence of fluid in the airway, usually blood or vomit, or both.
The record at N-4 of the Nurses’ Notes documents “incontinent blood tinged urine” at 0305 hours that is consistent with urinary incontinence (leakage of urine) or blood tinged urine if bladder infection is also present. Dark, concentrated urine in decreasing amounts (incontinent tinged urine) is also a prominant finding in patients with high blood sugar (hyperglycemia), including dehydration. Urinary dysfunction such as incontinence (leaking) of urine is a prominent finding in GBS patients due to autonomic abnormalities. Incontinence is loss of bladder control, and is also a very serious side effect of antipsychotic medications, such as Stemetil.
A-8 of the related record documents “patient was unconscious with respirations of approximately 30 and laboured”, that is consistent with dyspnea, being difficult or labored breathing. Dyspnea is breathlessness due to high filling pressures and pulmonary congestion/edema, i.e. shortness of breath, a smothering feeling, inability to get enough air, and suffocation. Breathing may become labored and difficult; labored breathing is the hallmark of respiratory distress and respiratory failure due to paralysis of the diaphragm. Breathing is affected by weakening the muscles of the chest wall and diaphragm; in these cases, mechanical ventilation is required immediately. Dyspnea should always be taken seriously.
A-1 documents “plantars upgoing bilaterally”. Submit that the plantar reflex is a hallmark of the Babinski sign, a test for signs of disease process in the motor neurons of the pyramidal tract. Initial drowsiness, bilateral plantar responses, and quadriparesis, is strong clinical evidence of central involvement consistent with drugs or toxins that affect the basal ganglia, thalmus or brain stem. Drugs such as Stemetil can impact the pyramidal tract. Babinski’s sign is also a prominent finding in Bickerstaff’s brainstem encephalitis (BBE), a variant of the Guillain Barre syndrome. Further, “limb weakness in GBS is nearly always bilateral” – (Parry, 1993).
The patient became apparently unresponsive, as evidenced at N-5, and went into respiratory distress, requiring ventilation for which she was transferred into ICU at 0320 hours, according to the record at N-3. The same record documents the time of the patient’s intubation by Dr. Jordan at 0325 hours, some 5 minutes later.
What I take to be the Ventilation Record at A-17 documents the arrival in the ICU of the hospital’s ventilatory therapist, Helene Studholme at 0330 hours, after being “called in for patient requiring ventilation”. From these records, it is clear that either the ventilatory therapist was not present at the time of the intubation procedure because she did not show up until 5 minutes later, or that the intubation did in fact take place at an earlier time, such as 0320 hours.
Notably, the record at A-24 documents a HR (heart rate) of 174 bpm at 0320 hours that is consistent with an awake intubation, (any suspicion of difficulty intubating, for any reason), marked by panic with awareness, resulting in an increased heart rate.
The Vital Signs Record at A-24 documents a heart rate of 174 bpm at 0320 hours that is consistent with trauma, while the Ventilation Record seen at A-16 documents a heart rate of only 126 within the same time frame, a significant difference, suggesting that the timeline for that event may have been altered by the Ventilatory Therapist to obfuscate iatrogenic trauma related injury. That A-17 documents the arrival in the ICU of the hospital’s ventilatory therapist, Helene Studholme at 0330 hours should be borne in mind.
The Vital Signs Record is a mechanical record with a run time, while the Ventilation Record is a handwritten account, marred by having been rewritten. Which method of recording is more likely to make copious errors or downplay an event by omission, or by telling lies?
There is nothing on record to suggest that anesthesia was or wasn’t given to prepare the patient for the intubation procedure. Submit, nothing entered can only infer “nothing done”. For the record, the earliest indication of shock is an increase in heart rate.
According to Dr. Jordan “the intubation proceeded uneventfully”, while N-2 of the record documents the ET (endotrachial tube) “pulled back 4 cm” at 0425 hours. From that record it seems clear that the endotrachial tube had been malpositioned for almost one full hour before the error was discovered by one of the nurses, as evidenced by the record at N-2, as to infer negligence on the part of the Dr. Jordan, including failure on his part to identify an incorrectly placed airway in a timely manner. Both myself and the patient’s foster brother were present to witness that event.
When an endotrachial tube is misplaced in the esophagus and misplacement is detected late, a compromise of the patient’s safety can be significant. Malpositioning of the ET tube can cause airway obstruction and may also result in tissue trauma and bleeding.
A-12 of the medical record documents a blood pressure of 163/117 bpm at 03:20 hours that by 0345 hours had dropped to 85/58 bpm following intubation, with an additional drop to 85/52 bpm by 0352 hours, over a span of some 7 minutes, as evidenced at N-2 in the Nurses’ Notes.
A-17 documents “being suctioned for moderate amounts of coffee-ground emesis by RN” at 0330 hours. Gastrointestinal bleeding due to stress ulceration is also an important complication in critically ill patients. GI bleeding is a medical emergency that was basically ignored by the healthcare providers, in this case.
The physician’s Lab Work Summary at A-19 documents the charting of a course of Hematology (bloodwork) and Coagulation. The same record documents a Fibrinogen level of 4.67 H (the normal range is 2.00-4.00). Elevated fibrinogen levels induce a state of hypercoagulability.
When blood protein is high, CSF usually clots because of the presence of increased fibrinogen. Serum fibrinogen levels in a safe range is <300 mg/dL. The plasma fibrinogen level appears to reflect disease activity in acute Guillain-Barre syndrome and is typically elevated at presentation. In fact, ongoing activity of Guillain-Barre syndrome may be reflected by a persistently elevated fibrinogen level. Further, elevated levels of fibrinogen may also be seen with TRAUMA of any kind.
A-19 documents a D-dimer test level of 1000 H. An increase in fibrinogen and d-dimer correlates with thrombotic activity suggestive of thrombosis. Thrombosis signifies the formation of blood clotting within vessels of the brain or neck. People who are suffering from a severe infection are more likely to develop dangerous blood clots, but inappropriate combinations of medications or treatment can sometimes be the worst offenders.
The Cardiac Index seen at A-18 documents the patient’s ventilation rate at 129 bpm (breaths per minute) at 0417 hours, with heart and breath rate increased. Increased heart and breath rate can suggest clinical insult, such as caused or worsened by medications, resulting in oxygen deprivation. The same record also documents the patient’s age at “55 years”, she was only 41 at the time of her death; can imply negligence, or even patient record swapping.
A-19 documents the aPTT (activated Partial Thromboplastin Time), a test used to determine the efficacy of various clotting factors used in the diagnosis of coagulation disorders documents the therapeutic range for heparin therapy at 60-100 seconds (23-35 is the normal). The time of that assessment was documented at 0400 hours. The aPTT is typically elevated in 90% of those with coagulopathy.
A-19 documents a “PLT ESTIMATE” – “MOD INCREASE” confirming an increase in platelet aggregation activity, blood platelets sticking together, indicating that blood thinners may be needed to prevent blood clots.
The ambulance call report seen at N-7, of the Nurses’ Notes documents that the patient was intubated and vented and that she was seen to be “stable”, but that she appeared to be “pale, dry and cool”. In patients with GBS, the skin may become pale and dry, and sweating may become reduced. Body temperature can also be marred by the effects of drug-induced temperature dysregulation, which can suppress sweating, causing central nervous system impairment, often resulting in an afebrile state. Cool, dry skin can also suggest late sepsis, usually associated with iatrogenic neglect.
Sepsis is also a frequent complication of Guillain Barre Syndrome. Severe sepsis may mimic Toxic Shock Syndrome. Sepsis refers to the presence of an infection, plus any two of these four criteria:
. Heart rate greater than 90 beats per minute
. Increased respiratory rate
. High or low white blood cell count
. Fever or low body temperature
. Visible symptoms of sepsis include nausea, vomiting and chills in the presence of an infection.
The record speaks for itself.
The most frequent sites of infection leading to sepsis are the lung, urinary tract, abdomen, and pelvis. In up to 30 percent of patients, however, a definite source of infection most often cannot be identified. The course of the disease is unpredictable. Some patients quickly deteriorate, while others suffer from varying degrees of organ dysfunction or begin to recover.
According to the Nurses’ Notes at N-1 of the record the patient was given Gravol 50 mg x 10 by paramedics at 0620 hours, while the record at N-7 with respect to medications documents “See Nsg Notes”. Gravol (dimenhydrinate) is contraindicated in lung disease and has also been reported to “mask the presence of underlying organic abnormalities and/or the toxic effects of other drugs”.
The record at A-8 and A-9 documents “Medi-Vac team were due to arrive at 0435″, while the Ambulance Call Sheet documents call received at 0620 hours, a significant difference. The record at N-7, documents “pulses X 4 good”; head and neck OK; chest OK; “abdomen OK”; pelvis OK; extremities OK.
A-1 of the record also documents “she died several days later with numerous metastatic lesions to her brain”. According to her death certificate, Arlene Berry died on "May 24th of 2000", the very same day she was transferred out to Sudbury. As to the cause of death, according to a Dr. Sauve in Sudbury, she died “meeting brain death criteria”.
NO attempt to diagnose was made at that time, or at all. No pathalogical reason was given for the declaration of brain death. No process of exclusion was undertaken without which a diagnosis of brain-death should never have been considered. NO explanation was offered to explain what can only be construed as a “fixed drug erruption” on the deceased’s right cheek.
It is believed that Arlene Berry’s death was deliberately provoked and that her eyes were taken by Drs. Sauve, and Adegbite at the Sudbury Regional Hospital, upon remote third party consent via her foster brother acting as a family contact, who was notified by phone. utilizing deception to obtain that consent, by-passing permission from Arlene Berry’s immediate family, ie, her de facto common-law spouse and her children.
From the information at hand, it seems clear that Drs.Sauve and Adegbite sought to open the way, under misleading conditions (influence of drugs, and metabolic disturbances) to organ donation from brain death. The diagnosis of brain death allows organ donation or withdrawal of life support. These doctors allowed this patient to die to achieve their nefarious ends.
Only unscrupulous clinicians might withhold medical treatment and attempt to influence the family in inappropriate ways such as this. Indeed, the fraudulent taking of the patient’s eyes in the manner in which it was done can only be construed as theft. The patient’s death can only be viewed as a medical homicide.
Certifying brain death to cover-up medical blunders or to increase organ donations constitutes murder.
Arlene Berry’s remains was returned to Kirkland Lake several days after family had been notified of her death only hours after her transfer Sudbury Regional Hospital. On seeing the deceased, her eyes were “sunken in appearance”, with swelling and distortion of the face, eyes, and lips, as was the case, marked by a rash-like redness resembling a sunburn with “blistering” wrinkles in the skin on her right cheek, in the area just below the right eye, consistent with a delayed hypersensitivity reaction, or fixed drug-eruption, evidenced by all who attended Arlene Berry’s viewing at the Monette Funeral Chapel in Kirkland Lake.
At a first meeting with the coroner held at the OPP Detachment in Kirkland Lake sometime in July of 2001, Dr. Barry A. McLellan, who was the Regional Supervising Coroner for northeastern Ontario at the time admitted to family that there was “no evidence on record to suggest matastasis”, meaning spread of cancer.
At a subsequent meeting between family and Dr. McLellan, he provided us with a view of a CT scan that was purportedly done in Sudbury, Ontario at the time Arlene’s death on May 24thy of 2000, although I suspect it may have been done following withdrawal of llife support. It shows multiple lesions of undetermined origin. The pathogenesis of these yet undetermined lesions remains unclear but a metabolic disorder seems the most plausible pathological factor.
Based on the patient’s belated CBC’s, the lesions are consistent with collections of purulent exudates (pus producing bacteria), suggested by an elevated Neutrophil count in the presence of an elevated WBC, and/or pockets of pooled blood, as suggested by an elevated Fibrinogen in the presence of an elevated D-dimer, a hallmark of thrombus formation, ie., blood clots. The enhancement is obviously due to infection, or blood pooling, or both.
No autopsy was performed, as I understand it, because the patient died “while under the care of a physician”. No appropriate period of observation and/or trial of therapy was ever undertaken. In fact, Arlene Berry was rushed to her death within five and one-half hours of her departure from the Kirkland and District Hospital to Sudbury Regional Hospital, some 210 miles away.
One might ask how much time did these medical dolts actually spend assessing the patient before taking away her life support? The speed at which they acted to hasten this death is nothing short of criminal.
Although many conditions can mimic brain death clinically upon examination, without excluding them you will KILL a person by homicide, or criminal negligence, despite the reversibility of brain damage.
Brain death is defined as the irreversible cessation of function of the entire brain with three specific criteria: 1) coma, 2) absent brainstem reflexes and 3) apnea. In addition to these clinical criteria, there are important prerequisites: 1) NO drug related intoxication or poisoning, 2) NO core temperature greater than 32 degrees Celsius, 3) clinical or neuroimaging evidence of acute central nervous system catastrophe and 4) absence of confounding medical conditions such as severe electrolyte, acid-base, or endocrine disturbances.
As a safeguard in determining brain death a number of tests need to be carried out every 6 hours and recorded. The physicians performing this determination must not be part of a transplantation team. In some cases, 48 to 72 hours or more is required to evaluate brain death and a repeat examination with observation up to an additional 24 hours is sometime needed. The length of time between serial examinations to declare brain death varies marginally from 6 to 72 hours. Notably, severe cases of GBS may mimic brain death.
Further, the Sudbury doctors involved were a part of an organ harvesting and transplantation team. It was Dr. Sauve who, utilizing deception, sought to obtain permission from a remote third party to obtain the victim’s eyes, without immediate family knowledge or consent.
With respect to the initial CT scan hereinbefore mentioned, according to the coroner’s expert “in the right occipital region there is a spot that measures less than 1 cm that is consistent in appearance with either a small hemorrhage or perhaps a small metastatic tumor”. He could only speculate. NO biopsy was done (a biopsy, is required for obtaining tissue for pathological confirmation of the diagnosis). The solitary lesion is also consistent in appearance with an abscess secondary to an occipital dermoid cyst, or early stage cerebritis during/after capsule formation in the early stage of abscess development. Rupture of a dermoid and leakage of a cyst contents into a ventricle or subarachnoid space may produce an epidymitis or meningitis respectively. Further, a single capsule can rupture resulting in the formation of multiple abscesses.
The bald truth is that localizing signs of brain tumor include a loss of vision on the side of an occipital neoplasm. Compare occipital abscess, or pyogenic brain abscess, usually of bacterial origin. Know that the occipital lobes interpret vision. Brain tumors are more solid/dense and therefore are usually associated with multi-focal deficits; tumors of the occipital lobe usually produce homonymous hemianopia or partial visual field deficits. Had the lesion been a recent tumor, there would have been onset visual misperception in half of one or both visual fields, with visual impairment and subsequent loss of vision with evolution, prior to hospital admission. That did not happen.
Know that even multiple brain abscesses may not cause focal deficit to suggest their presence. Non-neoplastic demyelinating processes of the brain with ring enhancing lesions and mass effect on MRI imaging, mimicking malignant brain tumors, are also a rare phenomena that was never considered. The radiologic appearance of demyelinating pseudotumors as contrast-enhancing masses that mimic tumor(s) is well documented, ie., “tumor-like” masses of demyelination, or “granulocytes that mimic brain tumors”.
Interestingly, granulocytes, which are cancer killing cells turn black as they die.
Further, with multiple abscesses or infection the meninges typically show a purulent exudate that obscures the sulci making radiographic appearance of microabscesses less visible, hence they are “not well opacified”. A brain abscess is generally caused by bacterial spread from an infection elsewhere in the body. Morbidity due to a brain abscess generally results from brain herniation due to mass effect, the result of iatrogenic neglect, or substandard care, or both.
No autopsy was performed in this case. Further, a family request for a formal inquest was also denied. Dr. McLellan concluded that Arlene Berry had died of “natural causes” suggestive of metastatic CA of the brain with multiple brain tumors after eliciting what can only be construed as a most questionable opinion from one of his fellow colleagues, believed to be associated with the Sunnybrook Health Sciences Centre, where McLellan spearheaded the North Telehealth Network. The medical record of Arlene Berry for May 23rd and 24th of 2000, tells a very different story from the opinion postulated. One might ask, why was so much evidence to the contrary ignored?
Eleven percent of mass lesions in cancer patients are not metastases; mass lesions that can masquerade as brain metastasis include abscess(20%) and granuloma (less common and mostly associated with myco-bacterial or fungal infection). The commonly observed deficits observed in CNS infection include weakness on one side of the body (hemiparesis), impaired speech production (dysphasia), visual field deficits (may or may not be present), and an inability to smoothly coordinate muscle movements, such as during walking (ataxia), which would cause a person to pull in one direction or another when walking,
Brain Tumor is often considered in the diagnosis of lesions demonstrated on brain computed tomography (CT) and/or magnetic resonance imaging (MRI). Brain tumors usually show abnormal densities on CT or altered signal intensities on MRI, mass effect, and sometimes contrast enhancement after the intravenous administration of contrast material. Lesions with these features, however, are not always brain tumors and establishing the diagnosis of a brain tumor is not always a straightforward process. Cerebrovascular diseases, demyelinating processes, inflammatory or infectious diseases and other miscellaneous diseases can show similar imaging findings.
Many non-neoplastic neurological diseases can mimic brain neoplasms on neuroimaging or on histological examination, including multiple sclerosis, stroke, pyogenic abscess, toxoplasmosis, tuberculosis, cysticercosis, fungal infections, syphilis, sarcoidosis, Bechet’s disease, radiation necrosis, venous thrombosis, Guillain Barre syndrome and others. Multiple intracerebral hematomas can also mimic brain metastases. West Nile virus encephalitis mimicking central nervous system metastases from small cell lung cancer is reported in the literature. Patients with a diagnosis of primary or metastatic brain tumor(s) associated with a CNS event should have a meticulous review of their history for other possible causes, especially iatrogenic causes.
The investigation and analysis of this case has been ongoing for 10 years with everything now pointing to Guillain Barre syndrome, with two second-guess possibilities in the differential which can not be ruled out, namely West Nile Virus, or Botulism, in that order. The differential diagnosis can be difficult, because the symptoms mimic those of Guillain-Barre syndrome. Further, fever in WNV apparently does not present in all cases. With GBS, fever is usually absent at onset. Although brain death mimickery is not an acute finding in WNV, it is with GBS, which also mimics brain death. That botulism may also mimic brain death needs always to be kept in mind. Yet, meningitis, encephalitis and Guillain-Barre syndrome remains undeniably the presentation in this case. I have to ask, is there a common denominator here?
For the record, meningoencephalitis (pronounced /mɛˌnɪŋɡɵ.ɛnˌsɛfəˈlaɪtɨs/, from Greek: meninges- membranes; enkephalos brain; and -itis inflammation) is a medical condition that simultaneously resembles both meningitis, which is an infection or inflammation of the meninges, and encephalitis, which is an infection or inflammation of the brain.
Meningitis and encephalitis are usually caused by viruses or bacteria. Less commonly, encephalitis can result from a bacterial infection, such as bacterial meningitis, or it may be a complication of other infectious diseases. Guillain-Barre is preceded by a viral or bacterial infection. Viral meningitis is the most common cause of aseptic meningitis, an inflammatory process involving the meninges in which usual bacterial etiologies cannot be identified. WNV season: May through October. A person with WNV-associated acute flaccid paralysis may present with or without fever or mental status changes, although fever is more common at onset. Also for the record, West Nile virus (WNV) can cause severe, potentially fatal neurological illnesses, which include encephalitis, meningitis, Guillain Barre syndrome, and anterior myelitis.
Questionable Opinion:
The anonymous author of an opinion sought by the coroner’s office (whose signature was erased) perceives himself to be expert in his field. Believed to be a neurosurgeon, perhaps the very same one who attended to Arlene Berry in Sudbury, this so called doctor is obviously lacking in diagnostic thoroughness. The bald truth is that specialists in a given field are not always expert in that field. In this case, his opinion remains unsubstantiated. He failed to provide any evidence whatsoever which might support a finding of metastatic CA of the brain. Further, a paltry CT scan does NOT provide conclusive proof of metastatic brain tumors. For that it takes a biopsy and in this case that was never done. Therefore the true nature of the lesions were never established. Nor does a CT provide conclusive proof of brain death. In fact the author who rendered the opinion suggesting metastatic cancer is pretty much off-the-wall; what one might expect from a “hand-picked, self-interest cash for comment” shill, or someone to be equated with a first year medical student whose opinion is highly questionable to say the least. The expert opinion even comes with a “disclaimer”.
The nameless author admits that his opinion “does not take into account all the facts and circumstances surrounding the patient’s death”, actually says it all since such a disclaimer can only raise doubt about the accuracy of the opinion rendered. The author bases his opinion on assumption, while ignoring the facts. Obviously he did not take the time to study the patient’s flawed medical record. Instead he opted to tailor or lard his report to justify the opinion that was, in his opinion , being sought by Dr. McLellan for the sake of expediency. This infers a blatant attempt by all concerned to obfuscate the truth.
A finding of possible meningitis with abscess of the brain and/or multiple intracerebral hematomas would have given more credibility to his opinion. In fact, some of the opinion expressed by the nameless author could also be used to support a finding of meningitis. There is absolutely nothing on record to support a finding of metastatic cancer of the brain, apart from a paltry CT, which offers absolutely NO evidence to support it. For the record, CBC is usually elevated in viral meningitis and there is initially a neutrophil predominance; polymorphonuclear leukocytes often predominated early in the course of such an infection.
Rapid deterioration is an invariable accompaniment of an untreated condition, in this case, an undiagnosed case of fulminant GBS with overlapping meningitis, in which rapid progress of the disease may actually be displaying a pronounced “blood-brain barrier breach”, characterized clinically by “rapid evolution”, the result of totally inappropriate treatment and/or medications which can breach blood-brain barrier integrity, ie. the drug Stemetil. Further, breakdown of the blood-brain barrier usually precedes inflammatory demyelination.
GBS is often associated with cerebrospinal meningitis and encephalitis. Coma in GBS is rare and is the symptom of cerebrospinal meningitis and encephalitis. The clinical manifestations of this condition included areflexia in the cranial and spinal nerves as well as apnoea. Cisterns may contain pus in cases of meningitis or other inflammatory conditions, such as sarcoid, or demyelination.
Any medical professional who, in rendering his opinion as to a cause of death, volunteers his unsolicited opinion as to another doctor’s conduct or standard of care in the face of overwhelming evidence to the contrary, finding in favour of his fellow colleague(s), invites being labeled retrospectively with the most nefarious motives.
Although two physicians with experience and expertise must be responsible for the declaration of brain death, and a neurologic condition capable of causing brain death is a mandatory prerequisite to the diagnosis of brain death, there are reports in the literature of conditions that mimic brain death or that provide examples of the mistaken diagnosis of brain death.
The clinical diagnosis of brain death occurred after the patient had received an IV tranquilizing agent and while still under the influence of morphine sulfate, an opiate narcotic, in this case.
GBS is one of the few neurological diseases whose clinical manifestations may mimic or appear to be identical to those in brainstem death, illustrating an extreme polyneuropathy.
Severe brainstem disease with loss of brainstem reflexes, labile vital signs and features of locked-in syndrome may also suggest West Nile Virus in the setting of GBS, however, GBS may rapidly evolve to a pseudo-coma-like state that resembles and can mimic brain death.
Further, know that Canadian standards “do not test function of the entire brain”, and there is sound evidence that many individuals who meet the clinical criteria of brain death continue to have some cortical, subcortical, or brain stem function. Many patients diagnosed as brain dead do not have hemodynamic collapse, they have physical findings such as bowel sounds, and are reported to have autonomic reflexes, tachycardia and hypertension, consistent with awareness and/or pain at the time of organ retrieval, suggesting a horrific death.
The clinical diagnosis of brain death, in this case, was made in the presence of metabolic derangements and endocrine abnormalities and constitutes an act of wanton and reckless disregard for human life. There have been many challenges to the several concepts of “brain death” and the means of their diagnosis worldwide (vide infra). Indeed, it seems that there is now an emerging consensus that “brain death diagnosed by any of the protocols in current use worldwide is not death.”
After the diagnosis of brain death, the focus of patient care shifts from interventions aimed at saving the patient’s life to interventions aimed at maintaining viability of potentially transplantable organs. Given that current clinical testing does not assess subcortical brain function, whole brain death cannot be conclusively identified at the bedside by using clinical criteria, and most certainly not on the basis of a paltry CT scan.
If the question is ischemic injury [brain damage caused by lack of blood/oxygen to part of the brain] you want an MRI and PET. For subsequent evaluation of brain injury, especially brain death, the CT is pretty much useless.
Many Ontario physicians actively involved in the identification of brain death, if the truth be known, are “unable to identify the requisite diagnostic components of brain death”, and/or are “unable to apply the criteria correctly”. Some physicians will take advantage of the situation to perpetrate a medical murder in order to harvest organs from potential donors, while others will simply declare “brain death” in order to avoid liability issues for medical wrongdoing.
Organ transplantation is premised on professional and public acceptance that the donor is dead and that the cessation of all brain function persists for an appropriate period of observation. The diagnosis of brain death allows organ donation or withdrawal of life support. The diagnosis of brain death is dependent upon the exclusion of certain medical conditions without which the diagnosis of brain-death cannot be considered and influence of medications is one of them.
Brain death declaration may be described as an esoteric creation of neurologists and neurosurgeons who are seeking to speed up death for the purposes of an organ transplants. In this case, the harried and hurried physicians simply used the questionable “brain death criteria”, based on a paltry CT after withdrawal of ventilatory support as a pretext to operate and remove the patient’s eyes while she was still very much alive.
For the record, eleven percent of mass lesions in cancer patients are not metastases; mass lesions that can masquerade as brain metastasis include abscess (20%) and granuloma (less common and mostly associated with mycobacterial or fungal infection). Patients with a diagnosis of primary or metastatic brain tumor(s) associated with a CNS event should have a meticulous review of their history for other possible causes. Take no one doctor’s word for anything. They cannot be trusted. There are too many bad apples in the system. If you have the resources, seek out a number of opinions via a medico-legal attorney. You might be surprised at what you find.
There are numerous reports of questionable ‘brain death’ declaration and at least two other cases are mentioned in the literature where “the criteria were deliberately misrepresented, or obfuscated in an attempt to retrieve an organ for transplantation”, as in this case. There are undoubtedly many other such cases, most of them cloaked in medical secrecy, hidden away from public view.
Brain death: resolving inconsistencies in the ethical declaration of death...
Status Code 0/ No Code
In my opinion, Arlene Berry’s death was premeditated, as evidenced by the physician’s documented patient status “Code 0″, seen at N-7 of the record and Dr. McLellan knowingly returned a false finding contrary to the Criminal Code of Canada for which he remains to be held to account. From the facts of this case it seems clear that this moral compass isn’t such a straight arrow after all.
Know that GBS is usually associated with prolonged length of ICU and hospital stay and requirement for rehabilitation, with significant use of health-care resources and cost implications is of itself sufficient motive for medical homicide.
The Arlene Berry Death Coverup!
In a letter to the College of Physicians and Surgeons of Ontario dated November 28, 2000, Dr. Jordan writes “discussed the situation with family members and a decision was made to intubate Ms. Berry”, while the Ambulance Call Report seen at N-7 documents an unsigned patient “Status Code 0″, or endorsement of what is more commonly termed a No Code. This is an order akin to a ‘DNR’ denying medical intervention, in this case by passing-the-buck together with all the possible blame.
Patient condition “Status Code Zero” taken from CMAJ articles, is used to describe a “dead” patient condition. The Yale Law Journal, Vol. 93, No. 2 (Dec., 1983), pp. 362-383, criticizes questionable hospital policies “that resort to third party adjudications in No-Code decision making”, and provides insight into the assigning of a “no-code order” instructing personnel “not to attempt resuscitation”, as in this case.
Looking over the patient’s chart it is clear that obtaining a ‘no code’ status in the face of immune mediated adversities by reason of Dr. Jordan’s and Dr. Spiller’s failure to recognize and treat an emergency situation accordingly, and by reason of Dr. Jordan’s failure to attend in a timely manner was the next essential step for these two negligent physicians in executing Arlene Berry’s death, either to spare the expense of treating her, or in order to avoid possible liability issues. In the alternative, Arlene Berry was targeted for euthanasia in order to harvest her eyes. No matter which way you look at it, she was murdered.
The Criminal Code of Canada regards euthanasia, whether passive or active, as culpable homicide, or murder: A culpable homicide is defined as murder “where the person who causes the death of a human being means to cause his death” (s. 229, Criminal Code of Canada). Unless the law has changed in recent years, euthanasia carries a fixed, minimum penalty of 10 years in prison. The ‘no code’ as evidenced in this case by a Patient Status “0″ was ordered by Drs. Jordan, and Spiller, without family knowledge or consent when the patient’s condition began to rapidly deteriorate following a whole chain of medical negligence, and substandard care that is nothing short of criminal.
With the help of Dr. Mark Spiller (who admitted Arlene Berry to the Kirkland and District Hospital on the evening of May 23rd), a cross-covering physician working the ER with Dr. Edward Jordan on a rotational basis, these two unscrupulous physicians were able to recruit two of their equally unscrupulous Sudbury colleagues to complete their dirty work at arms length. Interestingly, Dr. Spiller had been a local appointed coroner working under Dr. Barry McLellan at the time, and also a classmate of Dr. Stephane Sauve, one of the Sudbury doctors involved in the cover-up.
Although it is clear that Arlene Berry was transferred to Sudbury with ventilator support, and although Drs. Jordan and Spiller were aware of the need for emergency care and life support, after ordering it, they canceled it, using the secretive no code (Code 0) endorsement as a pretext for evoking a declaration of death and in fact waited for the patient’s death.
Within a few hours following her transfer from the Kirkland and District Hospital to the Sudbury Regional Hospital, Arlene Berry was declared as having met with ‘brain death criteria’ , while under the care of Drs. Stephane Sauve and Andrew Adegbite. Her remains were kept in Sudbury for several days prior to being returned to Kirkland Lake.
Withholding life sustaining treatment from an “undiagnosed” patient with concurrent hyperglycemia, hypokalemia and electrolyte abnormalities in combination with a severely paralyzed motor function and who is under the influence of sedative hypnotic and tranquilizing agents is of questionable legality. Death results from respiratory paralysis and subsequent asphyxiation. Brain death is also what happens when ventilator support is discontinued in patients with critical illness.
Turn off the respirator and in the natural course of affairs the patient dies from lack of oxygen. To practice euthenasia by withdrawing life support to a critically ill patient is a medical homicide ; to kill or destroy by preventing access of air or oxygen. An act of active euthenasia consists of killing someone; to do acts causing death, or by choosing not to act is also an act, which determines the course and the outcome of events. Turning off a respirator is a form of passive euthanasia that is sometimes practiced by doctors with a family’s consent. In this case, no such consent was ever given.
Passive euthenasia involves an allowing of “nature to take its course”. And that is exactly what Dr. Jordan had initially proposed to family. We were not impressed, opting instead for “aggressive treatment”.
Passive euthanasia also includes giving a patient large doses of morphine to control pain, in spite of the likelihood that the painkiller will suppress respiration and cause death. Such doses of painkillers have a dual effect of relieving pain and hastening death. That the patient had not been diagnosed as evidenced at A-3, should also be borne in mind.
Criminal negligence is defined as an act of wanton and reckless disregard for human life , in this case, causing death.
In looking over the coroner’s report, was this Dr. McLellan’s way of exonerating those responsible for Arlene Berry’s death in order to shield the local appointed coroner working under him at that time from liability? Or was it just a blatant attempt on his part to shield his fellow colleagues from absolute disgrace? Regardless of his motive, it clearly makes him an accomplice.
1. Dr. Sauve sought to open the way to organ donation from brain death under misleading conditions (influence of medications, and metabolic disturbances), further utilizing deception to obtain remote third party consent to harvest my wife’s eyes, bypassing permission from the immediate family, namely her de facto spouse and children. Interestingly, Dr. Sauve was a “classmate” of Dr. Mark Spiller, having attended the University of Toronto, Class of ’89. Dr. Sauve’s name apprears on the Clinical Investigator Inspection List (CLIIL) for Investigational New Drug Studies, and also on the Population Health Research Institute Canada Centre Information list, suggestive of perhaps some hidden agenda, either in the nature of influencing government spending for hospital funding, or some sinister plot involving population control by medical homicide, or both.
2. Suspected of theft of organs by harvesting from a living person by misrepresentation and accessory to medical homicide are: Adegbite, Andrew Babafunso Olanrewaju – Sudbury, ON – (CPSO#54992 ) and Sauve, Stephane Jean – Sudbury (CPSO# 61381); MDs with privileges at the Sudbury Regional Hospital – Laurentian Site.
3. Suspected of criminal negligence causing bodily harm, and liability murder in order to save face are Jordan, Edward Henry – Kirkland Lake, ON (CPSO#61732), and Spiller, Mark Arthur (CPSO#60977); cross-covering physicians working the ER at the Kirkland and District Hospital in Kirkland Lake, ON. In concert with the admitting physician, Dr. Mark Spiller, the decision was made by Dr. Edward Jordan to have the patient’s senses blunted with morphine and prepared for organ harvest using what is termed in medical jargon as the “slow code” in his absense. This is reflected by the record by the manner in which the patient was attended from the time of her admission to the Kirkland and District Hospital on May 23rd of 2000, to the time of her discharge and subsequent transfer out to Sudbury the following day, in the early hours of the morning on May 24th.
To allow or hasten a patient’s death to cover-up error or negligence or to obtain organs is reprehensible. It is nothing short of murder since such an act or omission which causes death carries the “intended” consequence of the act or omission, hence, the mens rea or criminal intent. Alternatively, all of the doctors and nurses named herein are guilty of criminal negligence causing death.
4. Suspected of conspiracy to conceal indictable offenses, and returning a false finding contrary to the Criminal Code of Canada is Dr. Barry Alexander McLellan who so happened to be the Regional Supervising Coroner at the time. Whats more, McLellan had been Dr. Spiller’s immediate supervisor, clearly a conflict of interest. A family request for a formal inquest was boldly denied by Dr. McLellan. Interestingly, Dr. McLellan’s office was in charge of administering the Human Tissue Gift Act and the Anatomy Act transplants. Dr. McLellan went on to become Ontario’s Chief Coroner and later discredited pathologist Dr. Charles Smith in order to turn suspicion away from his own faulty findings and sordid immorality. As of September 17, 2007, Dr. McLellan joined Sunnybrook Hospital in Toronto as its new CEO. It is not yet clear whether McLellan stepped down in order to seek refuge among his fellow equally contemptable colleagues, or if he was simply given the boot over the public disclosure of “systemic failure from 1981 to 2001″ uncovered in the office of the chief coroner associated with “oversight of death investigations” in Ontario.
This case is now a matter of public record. It has been widely reported and publicized through various Internet media, Topix forums as well as the Indymedia IMC throughout Canada, the USA, and the UK. The long standing silence of the doctors named herein confirms their active and ongoing concealment, which includes not only secrecy and deception, but also reticence and non-acknowledgment for their part in the Arlene Berry death cover-up.
ADDENDUM
Dr. de la Rocha had a vested interest in molecular mimicry and the West Nile Virus by reason of his affiliation with the “Canadian bioscience community”and in fact is a Co-author on the subject of estimating the “Prevalence of West Nile Virus Infection”. West Nile virus is like the flu.
Further, the focus of intense investigation of novel experimental approaches in treating cancer, ameba is a parasite in stealth candidly used to exploit the unsuspecting poor as human guinea pigs in the treatment of various cancers, still in the preliminary stages of experimental parasitology. The idea of using disease to fight disease became popular around the late nineties. Amoebas are used extensively in cell research for determining the relative functions and interactions of the nucleus and the cytoplasm.
An ameboma, or amebic granuloma is a tumor-like mass that occurs in amebiasis. In fact, amebomas are cancer’s closest known mimic. Cancer-suppressing protein is part of amoebas compass.
In Canada and the United States, amebiasis is a source of infectious cysts, most often found in immigrants. Further, many immigrant doctors who come to Canada have very low qualifications. Many of them have been exposed to malaria, parasites and many unfamiliar infectious diseases such as amebiasis. Amebiasis is also is found in people who have traveled to or who have come into contact with people from developing countries such as Mexico and in people who live or work in institutions or hospitals that have poor sanitary conditions, which pose health issues for all concerned.
Also, know that adenocarcinoma and amebic cysts present similarly as an “area of consolidation”. Presentation as a pulmonary nodule mimicking lung cancer is also common.
Routine bacterial cultures are usually “NEGATIVE” for pathogens, showing "No Growth", as in this case. Untreated patients may develop toxic megacolon. The use of opioids can lead to a rapid deterioration and colonic perforation.
Further, a change in the bacterial flora caused by a secondary bacterial (aerobic?) infection or the use of certain antibiotics may induce conversion from nonpathogenic to the active state (pathogenic) which causes the clinical disease.
Notably, certain combinations of medications, such as penicillin and sulfa-based anti-biotics can also cause the body’s immune system to react by overstimulation, steering the body’s already exhausted immune system, and/or volume depleted patient into dangerous waters; the very same process by which Guillain Barre syndrome (GBS) may also be triggered. Cipro and Septra DS have been implicated high on the order of major offenders in drug-induced GBS.
Dr. de la Rocha immigrated to Canada from Mexico where he graduated from the National Autonomous University of Mexico. Mexico is a hotbed for parasites and unfamiliar infectious diseases, such as amebiasis. Dr. de la Rocha is suspected of involvement in experimental virology, parasitology and/or of being the carrier, transmitter or purveyor of infectious diseases, either unwittingly, or by design.
de la Rocha has since moved from Timmins to Markham, Ontario.
Get the FACTS!
http://medicaries.webs.com/enigma.htm
A Medical Enigma
View the medical record of Arlene Berry
Guillain-Barré Syndrome: The Untold Story
Guillain–Barré syndrome
Guillain Barre syndrome (GBS)
Guillain-Barre Syndrome | A Solitary Confinement
GBS | Killer Nerve Disease
Pandemic & Human Guinea-pigs ?
 |
 |
|||||||||
|
||||||||||
Retrait de la rubrique Abitibi-Témis. (WTF!) Remplacement de la rubrique Éducation par Santé. Michaël Lessard [me contacter] [ ] |
||||||||||
 |
 |
|||||||||
 |
 |
 |
 |
G20 Special |  |
 |
 |
|
 |
 |
|
 |
We offer many independent reports and testimonies...
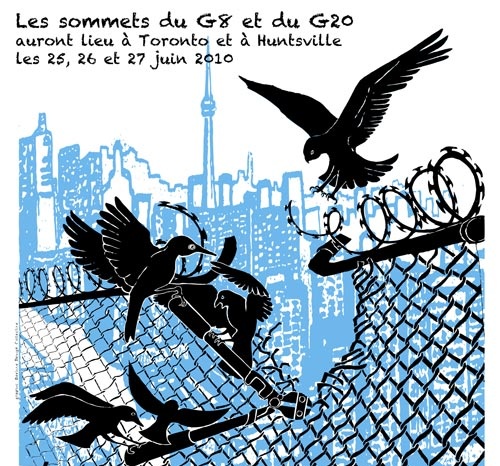
List of actions held during this "counter-summit" in Toronto You may also want to visit these alternative media in Toronto: G20 Alternative Media Centre http://2010.mediacoop.ca Media Co-op Toronto http://toronto.mediacoop.ca Toronto Community Mobilization www.attacktheroots.net |
 |
 |
 |
 |
 |
 |
 |
CMAQ: Vie associative |  |
 |
 |
|
 |
 |
|
 |
 Quebec City collective: no longer exist. Get involved ! |
 |
 |
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
Ceci est un média alternatif de publication ouverte. Le collectif CMAQ, qui gère la validation des contributions sur le Indymedia-Québec, n'endosse aucunement les propos et ne juge pas de la véracité des informations. Ce sont les commentaires des Internautes, comme vous, qui servent à évaluer la qualité de l'information. Nous avons néanmoins une
Politique éditoriale
, qui essentiellement demande que les contributions portent sur une question d'émancipation et ne proviennent pas de médias commerciaux.
This is an alternative media using open publishing. The CMAQ collective, who validates the posts submitted on the Indymedia-Quebec, does not endorse in any way the opinions and statements and does not judge if the information is correct or true. The quality of the information is evaluated by the comments from Internet surfers, like yourself. We nonetheless have an
Editorial Policy
, which essentially requires that posts be related to questions of emancipation and does not come from a commercial media.


